Introduction
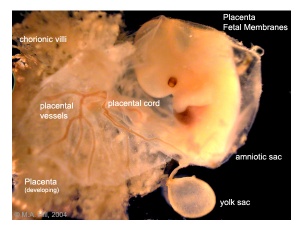
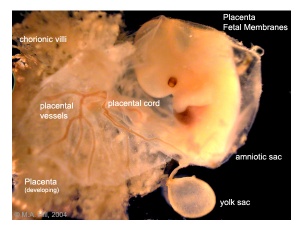
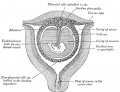
Human Placental Membranes
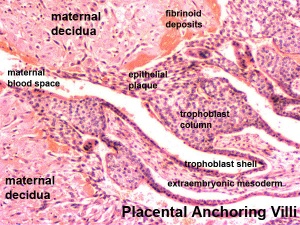
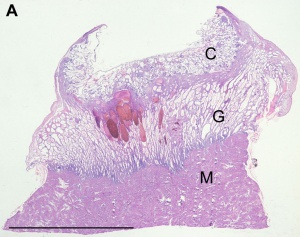
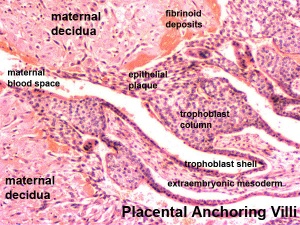
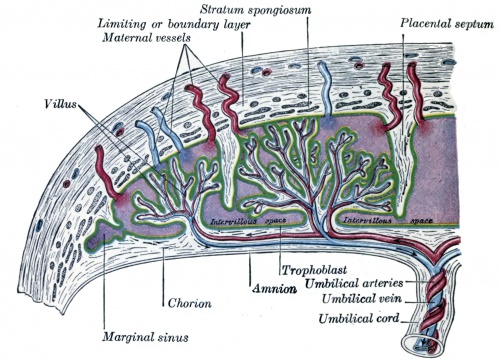
Placenta anchoring villi and Maternal decidua
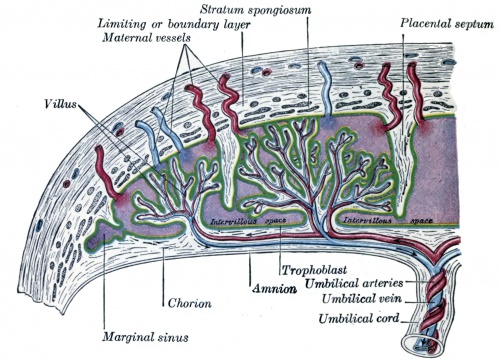
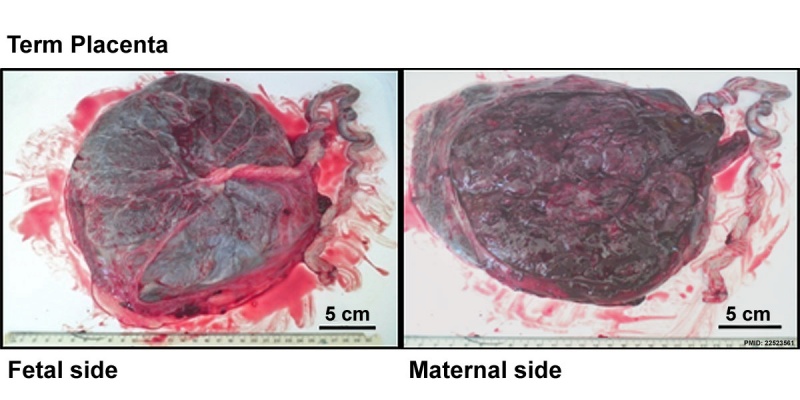
The placenta (Greek, plakuos = flat cake) named on the basis of this organs gross anatomical appearance. The placenta a mateno-fetal organ which begins developing at implantation of the blastocyst and is delivered with the fetus at birth. During that 9 month period it provides nutrition, gas exchange, waste removal, a source of hematopoietic stem cells, endocrine and immune support for the developing fetus.
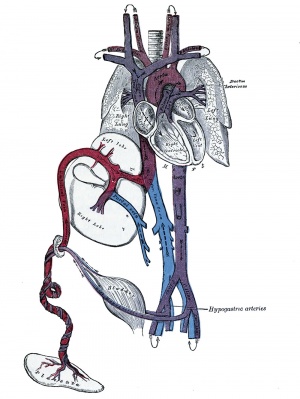
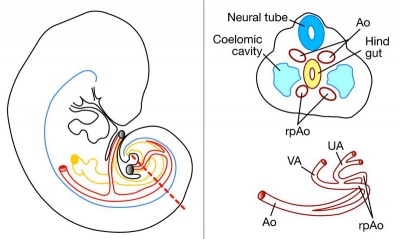
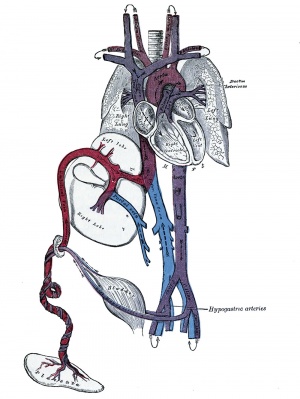
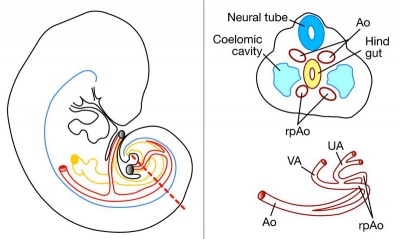
There are essentially 3 separate aortic/venous circulatory systems: umbilical, systemic and vitelline. The umbilical system is lost at birth, the vitelline contributes to the portal system and the systemic (embryonic) is extensively remodelled to form the mature cardiovascular system.
Nutrition is derived from about 100–150 maternal uterine spiral arteries located in the basal plate and the human term placenta is about 9 cm in diameter. There appears to also be differences in placentation (function) between the sexes.[1][2]
Some Recent Findings
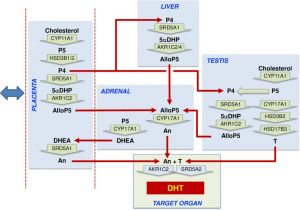
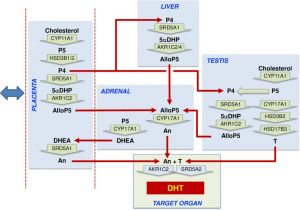
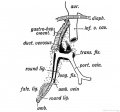
Model male second trimester androsterone synthesis
[3]
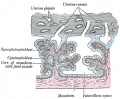
- Maternal platelets at the first trimester maternal-placental interface - Small players with great impact on placenta development[4] "In human pregnancy, maternal platelet counts decrease with each trimester, reaching a reduction by approximately ten percent at term in uncomplicated cases and recover to the levels of the non-pregnant state a few weeks postpartum. The time when maternal platelets start to occur in the early human placenta most likely coincides with the appearance of loosely cohesive endovascular trophoblast plugs showing capillary-sized channels by mid first trimester. At that time, platelets accumulate in intercellular gaps of anchoring parts of trophoblast columns and start to adhere to the surface of placental villi and the chorionic plate. This is considered as normal process that contributes to placenta development by acting on both the extravillous- and the villous trophoblast compartment. Release of platelet cargo into intercellular gaps of anchoring cell columns may affect partial epithelial-to-mesenchymal transition and invasiveness of extravillous trophoblasts as well as deposition of fibrinoid in the basal plate. Activation of maternal platelets on the villous surface leads to perivillous fibrin-type fibrinoid deposition, contributing to the shaping of the developing placental villi and the intervillous space. In contrast, excess platelet activation at the villous surface leads to deregulation of the endocrine activity, sterile inflammation and local apoptosis of the syncytiotrophoblast."
- FcRn, but not FcγRs, drives maternal-fetal transplacental transport of human IgG antibodies PNAS "Transport of IgG antibodies from the maternal to the fetal circulation is a key process for neonatal immunity, as neonates cannot sufficiently generate IgG antibodies to reach protective levels during the first months after birth. In humans and other primates, maternal to fetal transport of IgG antibodies is largely mediated through the placental tissue. FcRn has been previously identified as the major driver of IgG transplacental transport. Here we examine whether other receptors, such as FcγRs, also contribute to the maternal-fetal IgG transfer. By characterizing the Fc domain structure of paired maternal-fetal IgG samples and modeling transplacental IgG transport in genetically engineered mouse strains, we determined that FcRn, but not FcγRs, is the major receptor that mediates transplacental IgG transport."
- Review - Development of the human placenta[5] "The placenta is essential for normal in utero development in mammals. In humans, defective placental formation underpins common pregnancy disorders such as pre-eclampsia and fetal growth restriction. The great variation in placental types across mammals means that animal models have been of limited use in understanding human placental development. However, new tools for studying human placental development, including 3D organoids, stem cell culture systems and single cell RNA sequencing, have brought new insights into this field. Here, we review the morphological, molecular and functional aspects of human placental formation, with a focus on the defining cell of the placenta - the trophoblast."
- Alternative (backdoor) androgen production and masculinization in the human fetus[3] "Masculinization of the external genitalia in humans is dependent on formation of 5α-dihydrotestosterone (DHT) through both the canonical androgenic pathway and an alternative (backdoor) pathway. The fetal testes are essential for canonical androgen production, but little is known about the synthesis of backdoor androgens, despite their known critical role in masculinization. ...Instead, the data indicate that placental progesterone acts as substrate for synthesis of backdoor androgens, which occurs across several tissues. Masculinization of the human fetus depends, therefore, on testosterone and androsterone synthesis by both the fetal testes and nongonadal tissues, leading to DHT formation at the genital tubercle. Our findings also provide a solid basis to explain why placental insufficiency is associated with disorders of sex development in humans." Male genital genital abnormalities
- Associations Between the Features of Gross Placental Morphology and Birthweight[6] "The placenta plays a critical role in regulating fetal growth. Recent studies suggest that there may be sex-specific differences in placental development. The purpose of our study was to evaluate the associations between birthweight and placental morphology in models adjusted for covariates and to assess sex-specific differences in these associations. We analyzed data from the Stillbirth Collaborative Research Network's population-based case-control study conducted between 2006 and 2008, which recruited cases of stillbirth and population-based controls in 5 states. Our analysis was restricted to singleton live births with a placental examination (n = 1229). Characteristics of placental morphology evaluated include thickness, surface area, difference in diameters, shape, and umbilical cord insertion site. We used linear regression to model birthweight as a function of placental morphology and covariates. Surface area had the greatest association with birthweight; a reduction in surface area of 83 cm2, which reflects the interquartile range, is associated with a 260.2-g reduction in birthweight (95% confidence interval, -299.9 to -220.6), after adjustment for other features of placental morphology and covariates. Reduced placental thickness was also associated with lower birthweight. These associations did not differ between males and females. Our results suggest that reduced placental thickness and surface area are independently associated with lower birthweight and that these relationships are not related to sex." birthweight
- The human placental proteome secreted into the maternal and fetal circulations in normal pregnancy based on 4-vessel sampling[7] "Blood samples from the maternal radial artery and uterine vein and umbilical artery and vein were obtained during Template:Cesarean section in 35 healthy women with term pregnancy. Slow off-rate modified aptamer (SOMA) protein-binding technology was used to quantify 1310 known proteins. The uteroplacental and umbilical venoarterial concentration differences were calculated. Thirty-four proteins were significantly secreted by the placenta into the maternal circulation, including placental growth factor, growth/differentiation factor 15, and matrix metalloproteinase 12. There were 341 proteins significantly secreted by the placenta into the fetal circulation. Only 7 proteins were secreted into both the fetal and maternal circulations, suggesting a distinct directionality in placental protein release. We examined changes across gestation in the proteins found to be significantly secreted by the placenta into the maternal circulation using serial blood samples from healthy women. Among the 34 proteins secreted into the maternal circulation, 8 changed significantly across gestation. The identified profiles of secreted placental proteins will allow us to identify novel minimally invasive biomarkers for human placental function across gestation and discover previously unknown proteins secreted by the human placenta that regulate maternal physiology and fetal development."
|
| More recent papers
|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
- This search now requires a manual link as the original PubMed extension has been disabled.
- The displayed list of references do not reflect any editorial selection of material based on content or relevance.
- References also appear on this list based upon the date of the actual page viewing.
References listed on the rest of the content page and the associated discussion page (listed under the publication year sub-headings) do include some editorial selection based upon both relevance and availability.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References
Search term: Placenta Embryology | Placenta Development | Placentation | decidualization
|
| Older papers
|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
- Murine transcription factor Math6 is a regulator of placenta development[8] "The murine basic helix-loop-helix transcription (bHLH) factor mouse atonal homolog 6 (Math6) is expressed in numerous organs and supposed to be involved in several developmental processes. Characterization of the endogenous spatiotemporal Math6 expression during placenta development reveals that Math6 is essential for an ordered decidualization and an important regulator of the maternal-fetal endocrine crosstalk regulating endometrial trophoblast invasion and differentiation. The strongly disturbed vascularization observed in the maternal placenta appears as an additional consequence of the altered endocrine status and as the main cause for the general hemorrhagic crisis."
- S100P enhances the motility and invasion of human trophoblast cell lines[9] "S100P has been shown to be a marker for carcinogenesis where its expression in solid tumours correlates with metastasis and a poor patient prognosis. This protein's role in any physiological process is, however, unknown. Here we first show that S100P is expressed both in trophoblasts in vivo as well as in some corresponding cell lines in culture. We demonstrate that S100P is predominantly expressed during the early stage of placental formation with its highest expression levels occurring during the first trimester of gestation, particularly in the invading columns and anchoring villi. Using gain or loss of function studies through overexpression or knockdown of S100P expression respectively, our work shows that S100P stimulates both cell motility and cellular invasion in different trophoblastic and first trimester EVT cell lines. Interestingly, cell invasion was seen to be more dramatically affected than cell migration. Our results suggest that S100P may be acting as an important regulator of trophoblast invasion during placentation."
- Development of the Human Placenta and Fetal heart: Synergic or Independent?[10]The placenta is the largest fetal organ, and toward the end of pregnancy the umbilical circulation receives at least 40% of the biventricular cardiac output. It is not surprising, therefore, that there are likely to be close haemodynamic links between the development of the placenta and the fetal heart. Development of the placenta is precocious, and in advance of that of the fetus. The placenta undergoes considerable remodeling at the end of the first trimester of pregnancy, and its vasculature is capable of adapting to environmental conditions and to variations in the blood supply received from the mother. ... In pregnancies complicated by preeclampsia and/or fetal growth restriction, utero-placental malperfusion induces smooth muscle cells surrounding the placental arteries to dedifferentiate and adopt a proliferative phenotype. This change is associated with increased umbilical resistance measured by Doppler ultrasound, and is likely to exert a major effect on the developing heart through the afterload. Thus, both the umbilical and maternal placental circulations may impact on development of the heart."
- Hox genes in the allantois essential for proper extra-embryonic function in placental mammals[11] " Here, we provide evidence that this functional novelty is not exclusive to Hoxa13 but is shared with its neighboring Hoxa11 and Hoxa10 genes. We show that the extra-embryonic function of these three Hoxa genes stems from their specific expression in the allantois, an extra-embryonic hallmark of amniote vertebrates. Interestingly, Hoxa10-13 expression in the allantois is conserved in chick embryos, which are non-placental amniotes, suggesting that the extra-embryonic recruitment of Hoxa10, Hoxa11 and Hoxa13 most likely arose in amniotes, i.e. prior to the emergence of placental mammals."
- A transient placental source of serotonin for the fetal forebrain[12] "Serotonin (5-hydroxytryptamine or 5-HT) is thought to regulate neurodevelopmental processes through maternal-fetal interactions that have long-term mental health implications. It is thought that beyond fetal 5-HT neurons there are significant maternal contributions to fetal 5-HT during pregnancy but this has not been tested empirically. ...We uncovered a placental 5-HT synthetic pathway from a maternal tryptophan precursor in both mice and humans. This study reveals a new, direct role for placental metabolic pathways in modulating fetal brain development and indicates that maternal-placental-fetal interactions could underlie the pronounced impact of 5-HT on long-lasting mental health outcomes."
- Comparative systems biology of human and mouse[13] "We collected protein and mRNA expression data through shot-gun proteomics and microarray expression analysis of the highly vascular exchange region, microdissected from the human and mouse near-term placenta. Over 7000 ortholog genes were detected with 70% co-expressed in both species. Close to 90% agreement was found between our human proteomic results and 1649 genes assayed by immunohistochemistry for expression in the human placenta in the Human Protein Atlas. Interestingly, over 80% of genes known to cause placental phenotypes in mouse are co-expressed in human."
|
Reading

Spiegel and Casseri: De formato foetu liber singularis (Dedication dated 1626).
- Human Embryology (2nd ed.) Larson Chapter 7 p151-188 Heart, Chapter 8 p189-228 Vasculature
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapter 14: p304-349
- Before we Are Born (5th ed.) Moore and Persaud Chapter 12; p241-254
- Essentials of Human Embryology Larson Chapter 7 p97-122 Heart, Chapter 8 p123-146 Vasculature
- Human Embryology Fitzgerald and Fitzgerald Chapter 13-17: p77-111
Placental Classification
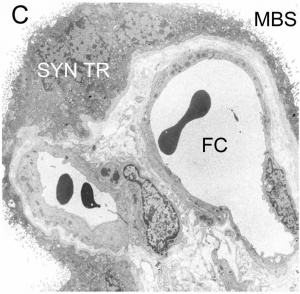
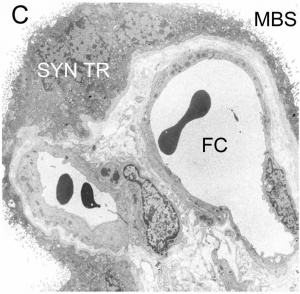
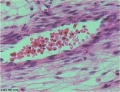
Haemomonochorial human placenta villi (EM) showing syncitiotrophoblast cells.
[14]Classification of placenta is on the basis of histological (microscopic) structural organization and layers between fetal and maternal circulation.
Three main groups:
- Haemochorial - placenta where the chorion comes in direct contact with maternal blood (human).
- Endotheliochorial - maternal endometrial blood vessels are bare to their endothelium and these comes in contact with the chorion (dogs, cats).
- Epitheliochorial - maternal epithelium of the uterus comes in contact with the chorion, considered as primitive (pigs, bovine).
The presence of these three differing types of placenta have also been used to describe the pattern mammalian evolution.
| Species Placental Comparison
|
Species Placental Forms and Types
| Order
|
Species
|
Placental Form
|
Maternal-fetal Interface
|
Maternal-fetal Membrane
|
| Primates
|
Ape, Human
|
Discoid
|
Villi
|
Haemochorial
|
| Rhesus
|
Bidiscoid
|
Villi
|
Haemochorial
|
| Tupaia
|
Bidiscoid
|
Labyrinth
|
Endotheliochorial
|
| Galago
|
Diffuse
|
Folded
|
Epitheliochorial
|
| Artiodactyla
|
| pig
|
Diffuse
|
Folded
|
Epitheliochorial
|
| sheep
|
Cotyledonary
|
Villi
|
Epithelio- & Syndesmo-chorial
|
| Cow, ?goat
|
Cotyledonary
|
Villi
|
Epitheliochorial
|
| Rodentia
|
| guinea pig
|
Discoid
|
Labyrinth
|
Haemomonochorial
|
| rat, mouse
|
Discoid
|
Labyrinth
|
Haemotrichorial
|
| Beaver
|
Discoid
|
Labyrinth
|
Hemodichorial
|
| Lagomorpha
|
rabbit
|
Discoid
|
Labyrinth
|
Haemochorial
|
| Carnivora
|
dog, cat
|
Zonary
|
Labyrinth
|
Endotheliochorial
|
| Perissodactyla
|
horse
|
Diffuse, spec.
|
Villi, "cups"
|
Epitheliochorial
|
| Cetacea
|
Whale, dolphin
|
Diffuse
|
Villi
|
Epitheliochorial
|
| Sirenia
|
Manatee
|
Zonary
|
Labyrinth
|
Haemochorial
|
| Chiroptera
|
bat
|
Discoid
|
Labyrinth
|
Endotheliochorial Occas. Hemochorial
|
| Insectivora
|
Europ. Mole
|
Discoid
|
Labyrinth
|
Haemochorial
|
| Scalopus
|
Diffuse
|
Labyrinth
|
Haemochorial
|
| Table based upon Comparative Placentation Links: placenta
|
|
Animal Model Comparison
| Postnatal Animal Models
|
mouse
|
rat
|
pig
|
| Pregnancy period (days)
|
18 – 21
|
21 – 23
|
110 – 118
|
| Placenta type
|
Discoidal, decidual
hemoendothelial choroidea
|
Discoidal, decidual
hemoendothelial choroidea
|
Epitheliochorial
|
| Litter size
|
6 – 12
|
6 – 15
|
11 – 16
|
| Birth weight (g)
|
0.5 – 1.5
|
3 – 5
|
900 – 1600
|
| Weaning weight male/female (g)
|
18 – 25/16 – 25
|
55 – 90/45 – 80
|
6000 – 8000
|
| Suckling period (days)
|
21–28
|
21
|
28–49
|
| Solid diet beginning (days)
|
10
|
12
|
12 – 15
|
| Puberty male/female (week)
|
4 – 6/5
|
6/6 – 8
|
20 – 28
|
| Life expectancy (years)
|
1 - 2
|
2 - 3
|
14 – 18
|
| Table data - Otis and Brent (1954)[15] Links: timeline
|
| Male Placenta?
|
| Well not exactly, but close. In vertebra and in placental mammals embryonic development is associated with the mother (maternal). The exception to this rule occurs in seahorses (syngnathidae) where the male has a "uterus", a special pouch (brood pouch), where deposited eggs embed in depressions of the pouch interior lining. This pouch also has "placental" functions serving as aeration, protection, osmoregulation and nutrition for the egg development. (More? PMID 23213429)
|
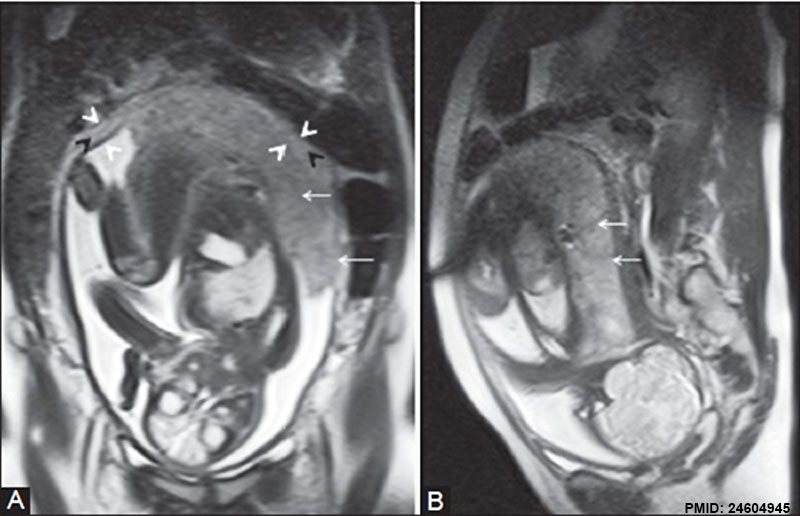
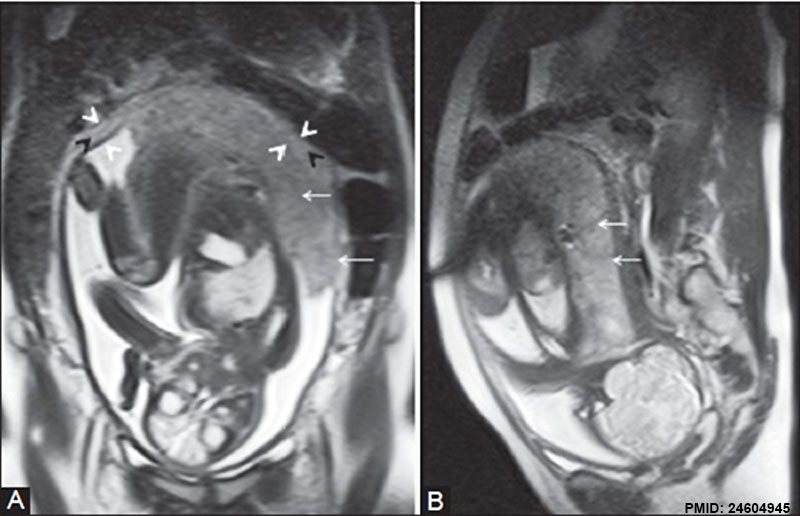
Placenta MRI (37 weeks)[16]
Placenta located at the upper segment of uterus.
Placental Villi Blood Vessels
Some of the following data is from a histological study of human placental villi.[18]
- macrophage-like cells first cells to differentiate at day 21 (post-conception) from mesenchymal precursors.
- haemangioblastic cell cords (angiogenic cell cords, ACC) at day 21 (post-conception) also from mesenchymal cells, are the precursors of the capillary endothelium and haematopoietic stem cells
- pericytes form later and are a third cell population derived from the mesenchymal cells
- first main vascular patterns grow towards the longitudinal axis of the developing villi
- capillary basal lamina cannot be detected earlier than in the third trimester
- third trimester - fetal villous angiogenesis occurs by proliferation of the existing endothelium and pericytes rather than through haemangioblastic cells.
Fetal Circulation
| Placental
|
Systematic
|
|
|
Human Villi Timeline
The placental vill development data below is based upon a recent immunochemistry confocal laser scanning microscope (CLSM) study.[19] Note that the paper uses clinical gestational age (GA) from last menstrual period (LMP) and has been corrected for post-conception (fertilization) age, approximately 14 days later.
Placenta Villi Timeline
| Fertilization Age
(weeks)
|
Gestational Age
(weeks)
|
Vessel Lumen Diameter
(range in microns)
|
Features
|
| 3 to 4
|
5 and 6
|
10 - 15
|
- complex network of cords and vessels with redundant connections
- network comprises mainly cords already connected together
- vessels and cords are connected to each other without any interruptions
- chorionic villus dominated by this network of vascular elements
- vessels and cords (centrally and peripherally) contact overlying trophoblastic layer
|
| 5 to 6
|
7 and 8
|
10 - 26
|
- villi dominated by capillary network of vessels and cords
- capillary network contains more vessels than cords
- chorionic villus tip - regular small branched off (mesenchymal) chorionic villi are present containing CD31 positive cells
|
| 7 to 8
|
9 and 10
|
60 - 75 two central vessels
26 - 34 capillary network
|
- villi have two large centrally located vessels
- surrounded and connected to a peripheral capillary network
- capillary network contains vessels with a lumen in tight contact with overlying trophoblastic layer
- villous projections also contain blind ending capillary sprouts
|
| 9 to 10
|
11 and 12
|
70 - 90 two central vessels
26 - 34 capillary network
|
- immature intermediate villi characterized by two large vessels surrounded by a capillary network
- capillary network has few cords
- blind ending capillary sprouts off the capillary network
|
| Term
|
|
|
Terminal villi
- have an extensive surface area >10 m2
- small calibre (40 – 100 µm)
|
| Table data[19] Paper uses clinical gestational age (GA) table corrected also for post-conception (fertilization) age.
|
CD31 - (PECAM-1, Platelet Endothelial Cell Adhesion Molecule) is a cluster of differentiation molecule found on endothelial and other blood cells.
Trophoblast Cells
Following implantation the initial trophoblast cells can differentiate into 2 pathways:
- Extravillous - cytotrophoblastic cells proliferate and differentiate into an invasive phenotype that invade (interstitial trophoblast) the maternal decidual stroma and the spiral arteries (endovascular trophoblast) of the myometrium.
- Villous - cytotrophoblastic cells proliferate and fuse to form the multi-nucleated syncytiotrophoblast cells that form the outer surface of the fetal placental villi.
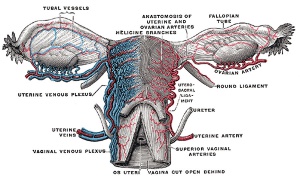
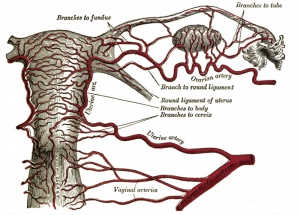
Maternal Blood Flow
Maternal blood pressure normally decreases or remains unchanged during pregnancy while both cardiac output and vascular volume are increased. Uterine blood flow changes are principally due to a decrease in uterine vascular resistance. There is also an associated structural enlargement of both the uterine arterial and venous trees, reduced vascular tone (vasodilation) and placenta development.
Uteroplacental blood flow (UPBF) was historically measured by a number of different mathematical calculations and probe methods, currently the method involves transvaginal doppler ultrasonography.
In human singleton pregnancies, uteroplacental blood flow (UPBF) begins at 20–50 ml/min and increases (linearly) to 450–800 ml/min, with twin pregnancy values in excess of 1 l/min.[20]
Uterine Artery Diameter
The following data is from a study of 18 pregnant women using ultrasound and doppler analysis of the uterine artery.[21]
- GA week 21 doubled (from 1.4 to 2.8 mm).
- GA week 21 to 30 remained constant (2.9mm).
- GA week 30 to 36 increased (to 3.4 mm).
Uterine artery mean flow velocity also increased nearly eight times from non-pregnant (8.4 cm/second) to GA week 36 (61.4 cm/second).
Arcuate and Radial Arteries
These branches from the paired uterine arteries also remodel enlarging in lumen diameter between 25 to 220% with either no change or an increase in wall thickness. Arcuate arteries also elongate either by longitudinal growth or by the progressive straightening of these coiled vessels.
- Links: ultrasound | cardiovascular
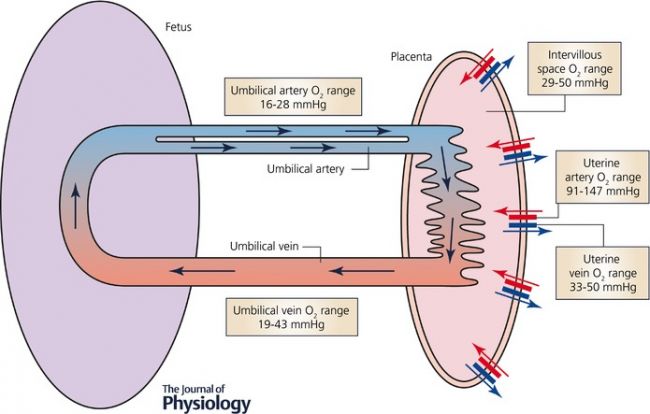
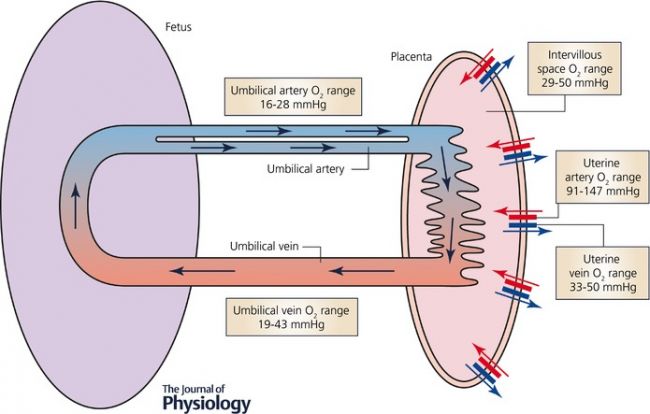
Blood Oxygen Levels
Maternal and Fetal Placental Circulations[22]
Showing the major compartments and published attributed in vivo oxygen values.
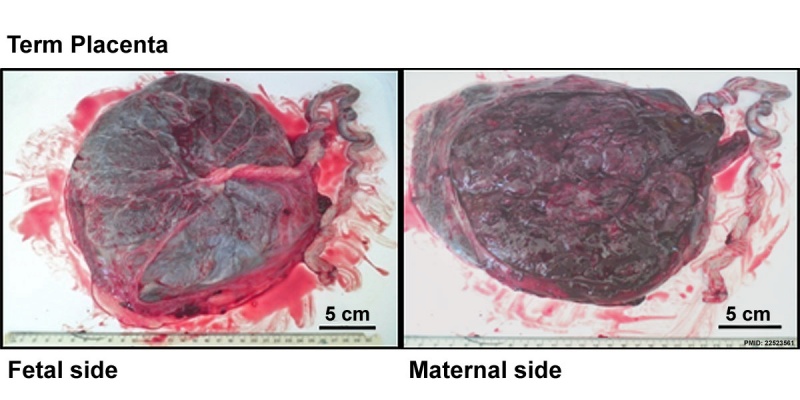
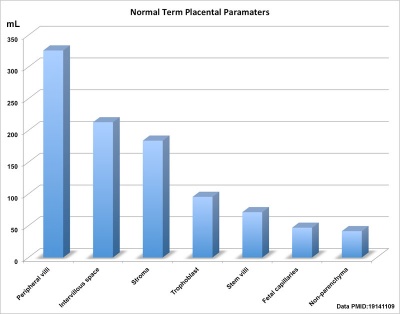
Term Placenta Measurements
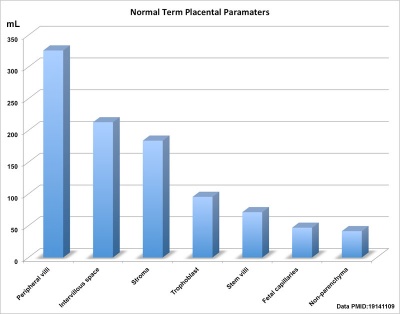
Human term placental volumes sorted by size (from table).
There are a variety of diagnostic and morphological measurements that can be made of the placenta during pregnancy and at term.
Simple measurements of overall placental diameter, thickness and volume:
- placental diameter - is measured in the transverse section by calculating the maximum dimensions of the chorionic surface.
- placental thickness - is measured at its mid-portion from the chorionic plate to the basilar plate, on a longitudinal plane (less than 4 cm at term). Excludes any abnormalities (fibroids, myometrial contractions, or venous lakes). The placental thickness approximates in millimeters to the weeks of gestation.
- placental volume - is measured by a range of different methods and calculations, more recently with three-dimensional ultrasound.
Detailed morphometric indices at term of placental composition, villous capillarization and the mean cross-sectional areas of peripheral villi and capillaries, data from a study sample of 15 normal placenta (mean placental volume, 652 ml).[23][24]
Term Placenta Measurements
| Variable
|
Unit
|
Placenta (mean, n = 15)
|
| Intervillous space
|
mL
|
213
|
| Stem villi
|
mL
|
71.4
|
| Peripheral villi
|
mL
|
326
|
| Trophoblast
|
mL
|
95.5
|
| Stroma
|
mL
|
184
|
| Fetal capillaries
|
mL
|
46.9
|
| Non-parenchyma
|
mL
|
41.5
|
| Peripheral villi
|
km
|
89.2
|
| Fetal capillaries
|
km
|
310
|
| total surface area villi
|
µm2
|
3700
|
| total surface area capillary
|
µm2
|
150
|
| Capillaries
|
mL mL-1
|
0.147
|
| Length ratio
|
km km-1
|
3.6
|
| Table data[24]
|
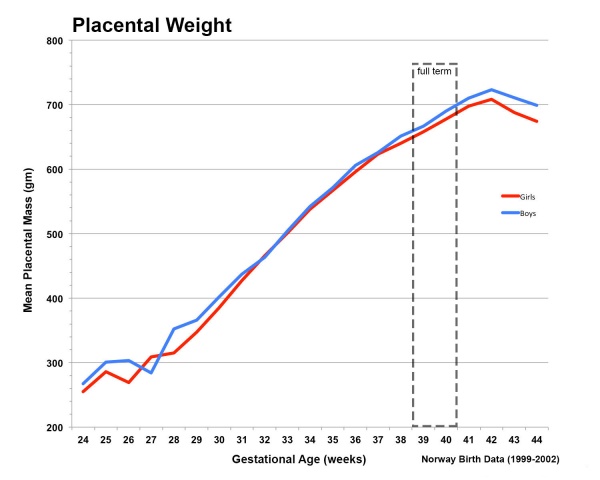
Placental Weight
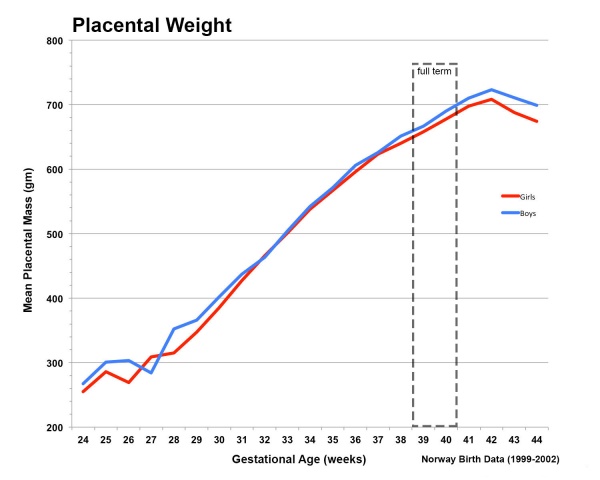
Fetal Placental weight growth[25]
Placental Factors
As the placenta develops it becomes the source of many different factors (hormones, growth factors) and also has the ability to metabolise both maternal and fetal factors.
Placental Growth Factor
(PGF, PLGF) A growth factor of the vascular endothelial growth factor (VEGF) family, released from the placental trophoblast cells and other sources that stimulates blood vessel growth. See review.[26]
- Links: OMIM601121 | Search PubMed
Insulin/insulin-like Growth Factor
- IGF1 and IGF2 are both synthesized in the placenta and the fetus.
- IGF1 present in syncytiotrophoblast and cytotrophoblast at all stages.
- IGF2 not found in the syncytiotrophoblasts.
- IGF2 expression in the villous and extravillous cytotrophoblasts in the first trimester becomes undetectable at term.
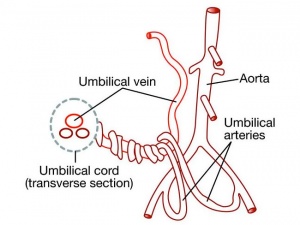
Placental Arteries and Vein
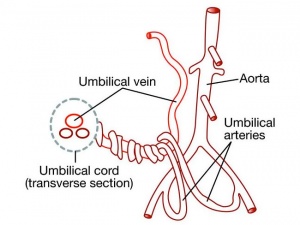
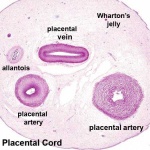
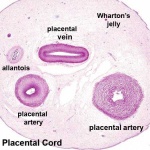
Placental Cord Histology
Placental cord cross-section
- Links: Placenta - Cord | Placenta - Histology
Placental Abnormalities

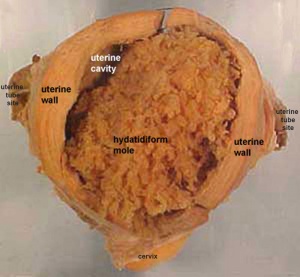
Historic model of placenta previa
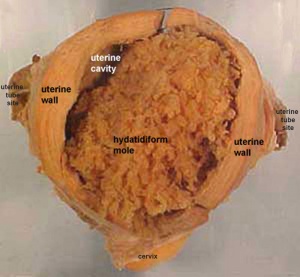
Hydatidiform mole pathology
Note there is also a specific page covering the topic of placental abnormalities.
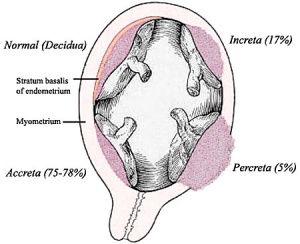
- Placenta Accreta - abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- Placenta Increta - occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
- Placenta Percreta - placental villi penetrate myometrium and through to uterine serosa.
- Placenta Previa - In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies. In the third trimester and at term, abnormal bleeding can require cesarian delivery and can also lead to Abruptio Placenta. Ultrasound screening programs during 1st and early 2nd trimester pregnancies now include placental localization. Diagnosis can also be made by transvaginal ultrasound.
- Vasa Previa - (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). This occurs normally in 1:2500-5000 pregnancies and leads to complications similar too those for Placenta Previa.Type II is defined as the condition where the fetal vessels are found crossing over the internal os connecting either a bilobed placenta or a succenturiate lobe with the main placental mass. Some recent evidence of successful in utero laser ablation of type II vasa previa at 22.5 weeks of gestation.
- Abruptio Placenta - a retroplacental blood clot formation, abnormal hemorrhage prior to delivery.
- Chronic Intervillositis - (massive chronic intervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
- Hydatidiform mole - placental tumor with no embryo development. Several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor. Many of these tumours arise from a haploid sperm fertilizing an egg without a female pronucleus (the alternative form, an embryo without sperm contribution, is called parthenogenesis). The tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
- Links: Placenta - Abnormalities
Placental Cord Abnormalities
There are few abnormalities associated with umbilical cord development, other that abnormally short or long cords, which in most cases do not cause difficulties. In some cases though, long cords can wrap around limbs or the fetus neck, which can then restrict blood flow or lead to tissue or nerve damage, and therefore effect develoment.
- Cord knotting - can also occur (1%) in most cases these knots have no effect, in some cases of severe knotting this can prevents the passage of placental blood.
- Cord torsion - Rare event where even without knot formation can also affect placental blood flow, even leading to fetal demise.
- Links: Placenta Cord Development | Placenta - Abnormalities | WebPath - umbilical cord knot 1 | WebPath - umbilical cord knot 2 | WebPath - Pseudoknot of umbilical cord, gross | WebPath - Torsion of umbilical cord, gross | WebPath - Torsion of umbilical cord, with fetal demise, gross
Placental Infections
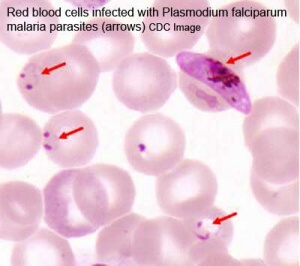
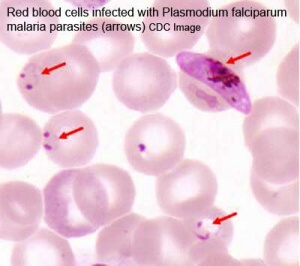
Malaria (plasmodium falciparum)
- Several infective agents may cross into the placenta from the maternal circulation, as well as enter the embry/fetal circulation. The variety of bacterial infections that can occur during pregnancy is as variable as the potential developmental effects, from virtually insignificant to a major developmental, abortive or fatal in outcome.
- Pregnant women have an increased susceptibility to malaria infection. Malarial infection of the placenta by sequestration of the infected red blood cells leading to low birth weight and other effects. There are four types of malaria caused by the protozoan parasite Plasmodium falciparum (main), Plasmodium vivax, Plasmodium ovale, Plasmodium malariae). This condition is common in regions where malaria is endemic with women carrying their first pregnancy (primigravida).
- Links: malaria | Viral | Bacterial
Placental Pathology
- Chronic Villitis - can occur following placental infection leading to maternal inflammation of the villous stroma, often with associated intervillositis. The inflammation can lead to disruption of blood flow and necrotic cell death.
- Massive Chronic Intervillositis (MCI) - maternal blood-filled space is filled with CD68-positive histiocytes and an increase in fibrin, occuring more commonly in the first trimester.
- Meconium Myonecrosis - prolonged meconium exposure leads to toxic death of myocytes of placental vessels (umbilical cord or chorionic plate).
- Neuroblastoma - a fetal malignancy that leads to an enlarged placenta, with tumor cells in the fetal circulation and rarely in the chorionic villi.
- Thrombophilias - (protein C or S deficiency, factor V Leiden, sickle cell disease, antiphospholipid antibody) can generate an increased fibrin/fibrinoid deposition in the maternal or intervillous space, this can trap and kill villi.
Comparative Placentation
The usual mouse model does not reflect human placentation in structure or function. Mouse does not synthesise estrogen not (Hyperglycosylated) chorionic gonadotropin.
The Comparative Placentation website has been available online for many years providing valuable information about placentation in a wide range of species. The site was developed by Dr Kurt Benirschke, a longstanding expert in the field.[27][28] Dr Kurt Benirschke retired in 1994 and continued to develop and maintain the website (that is still available) until 2012, but it has not been updated since that time.
- Links: homepage | index | glossary
References
- ↑ Brown ZA, Schalekamp-Timmermans S, Tiemeier HW, Hofman A, Jaddoe VW & Steegers EA. (2014). Fetal sex specific differences in human placentation: a prospective cohort study. Placenta , 35, 359-64. PMID: 24720894 DOI.
- ↑ Rosenfeld CS. (2015). Sex-Specific Placental Responses in Fetal Development. Endocrinology , 156, 3422-34. PMID: 26241064 DOI.
- ↑ 3.0 3.1 O'Shaughnessy PJ, Antignac JP, Le Bizec B, Morvan ML, Svechnikov K, Söder O, Savchuk I, Monteiro A, Soffientini U, Johnston ZC, Bellingham M, Hough D, Walker N, Filis P & Fowler PA. (2019). Alternative (backdoor) androgen production and masculinization in the human fetus. PLoS Biol. , 17, e3000002. PMID: 30763313 DOI.
- ↑ Guettler J, Forstner D & Gauster M. (2021). Maternal platelets at the first trimester maternal-placental interface - Small players with great impact on placenta development. Placenta , , . PMID: 34920861 DOI.
- ↑ Turco MY & Moffett A. (2019). Development of the human placenta. Development , 146, . PMID: 31776138 DOI.
- ↑ Freedman AA, Hogue CJ, Marsit CJ, Rajakumar A, Smith AK, Goldenberg RL, Dudley DJ, Saade GR, Silver RM, Gibbins KJ, Stoll BJ, Bukowski R & Drews-Botsch C. (2019). Associations Between the Features of Gross Placental Morphology and Birthweight. Pediatr. Dev. Pathol. , 22, 194-204. PMID: 30012074 DOI.
- ↑ Michelsen TM, Henriksen T, Reinhold D, Powell TL & Jansson T. (2018). The human placental proteome secreted into the maternal and fetal circulations in normal pregnancy based on 4-vessel sampling. FASEB J. , , fj201801193R. PMID: 30335547 DOI.
- ↑ Böing M, Brand-Saberi B & Napirei M. (2018). Murine transcription factor Math6 is a regulator of placenta development. Sci Rep , 8, 14997. PMID: 30301918 DOI.
- ↑ Tabrizi MEA, Lancaster TL, Ismail TM, Georgiadou A, Ganguly A, Mistry JJ, Wang K, Rudland PS, Ahmad S & Gross SR. (2018). S100P enhances the motility and invasion of human trophoblast cell lines. Sci Rep , 8, 11488. PMID: 30065265 DOI.
- ↑ Burton GJ & Jauniaux E. (2018). Development of the Human Placenta and Fetal Heart: Synergic or Independent?. Front Physiol , 9, 373. PMID: 29706899 DOI.
- ↑ Scotti M & Kmita M. (2012). Recruitment of 5' Hoxa genes in the allantois is essential for proper extra-embryonic function in placental mammals. Development , 139, 731-9. PMID: 22219351 DOI.
- ↑ Bonnin A, Goeden N, Chen K, Wilson ML, King J, Shih JC, Blakely RD, Deneris ES & Levitt P. (2011). A transient placental source of serotonin for the fetal forebrain. Nature , 472, 347-50. PMID: 21512572 DOI.
- ↑ Cox B, Kotlyar M, Evangelou AI, Ignatchenko V, Ignatchenko A, Whiteley K, Jurisica I, Adamson SL, Rossant J & Kislinger T. (2009). Comparative systems biology of human and mouse as a tool to guide the modeling of human placental pathology. Mol. Syst. Biol. , 5, 279. PMID: 19536202 DOI.
- ↑ Carter AM & Enders AC. (2004). Comparative aspects of trophoblast development and placentation. Reprod. Biol. Endocrinol. , 2, 46. PMID: 15236656 DOI.
- ↑ Otis EM and Brent R. Equivalent ages in mouse and human embryos. (1954) Anat Rec. 120(1):33-63. PMID 13207763
- ↑ Varghese B, Singh N, George RA & Gilvaz S. (2013). Magnetic resonance imaging of placenta accreta. Indian J Radiol Imaging , 23, 379-85. PMID: 24604945 DOI.
- ↑ Hempstock J, Cindrova-Davies T, Jauniaux E & Burton GJ. (2004). Endometrial glands as a source of nutrients, growth factors and cytokines during the first trimester of human pregnancy: a morphological and immunohistochemical study. Reprod. Biol. Endocrinol. , 2, 58. PMID: 15265238 DOI.
- ↑ Demir R, Kaufmann P, Castellucci M, Erbengi T & Kotowski A. (1989). Fetal vasculogenesis and angiogenesis in human placental villi. Acta Anat (Basel) , 136, 190-203. PMID: 2481376
- ↑ 19.0 19.1 Lisman BA, van den Hoff MJ, Boer K, Bleker OP, van Groningen K & Exalto N. (2007). The architecture of first trimester chorionic villous vascularization: a confocal laser scanning microscopical study. Hum. Reprod. , 22, 2254-60. PMID: 17545656 DOI.
- ↑ Osol G & Mandala M. (2009). Maternal uterine vascular remodeling during pregnancy. Physiology (Bethesda) , 24, 58-71. PMID: 19196652 DOI.
- ↑ Palmer SK, Zamudio S, Coffin C, Parker S, Stamm E & Moore LG. (1992). Quantitative estimation of human uterine artery blood flow and pelvic blood flow redistribution in pregnancy. Obstet Gynecol , 80, 1000-6. PMID: 1448242
- ↑ Nye GA, Ingram E, Johnstone ED, Jensen OE, Schneider H, Lewis RM, Chernyavsky IL & Brownbill P. (2018). Human placental oxygenation in late gestation: experimental and theoretical approaches. J. Physiol. (Lond.) , 596, 5523-5534. PMID: 29377190 DOI.
- ↑ Mayhew TM, Jenkins H, Todd B & Clifton VL. (2008). Maternal asthma and placental morphometry: effects of severity, treatment and fetal sex. Placenta , 29, 366-73. PMID: 18328557 DOI.
- ↑ 24.0 24.1 Mayhew TM. (2009). A stereological perspective on placental morphology in normal and complicated pregnancies. J. Anat. , 215, 77-90. PMID: 19141109 DOI.
- ↑ Thompson JM, Irgens LM, Skjaerven R & Rasmussen S. (2007). Placenta weight percentile curves for singleton deliveries. BJOG , 114, 715-20. PMID: 17516963 DOI.
- ↑ De Falco S. (2012). The discovery of placenta growth factor and its biological activity. Exp. Mol. Med. , 44, 1-9. PMID: 22228176 DOI.
- ↑ Benirschke K. (1998). Remarkable placenta. Clin Anat , 11, 194-205. PMID: 9579593 <194::AID-CA8>3.0.CO;2-T DOI.
- ↑ Benirschke K. (2002). Placentas, peccaries, and pathologists: reminiscences of Kurt Benirschke on his career: an interview with Rebecca N. Baergen. Int. J. Gynecol. Pathol. , 21, 289-300. PMID: 12068178
Reviews
Raeside JI. (2017). A Brief Account of the Discovery of the Fetal/Placental Unit for Estrogen Production in Equine and Human Pregnancies: Relation to Human Medicine. Yale J Biol Med , 90, 449-461. PMID: 28955183
Ferner K & Mess A. (2011). Evolution and development of fetal membranes and placentation in amniote vertebrates. Respir Physiol Neurobiol , 178, 39-50. PMID: 21470579 DOI.
Riquelme G. (2011). Review: Placental syncytiotrophoblast membranes--domains, subdomains and microdomains. Placenta , 32 Suppl 2, S196-202. PMID: 21272934 DOI.
Cartwright JE, Fraser R, Leslie K, Wallace AE & James JL. (2010). Remodelling at the maternal-fetal interface: relevance to human pregnancy disorders. Reproduction , 140, 803-13. PMID: 20837731 DOI.
Ferner K & Mess A. (2011). Evolution and development of fetal membranes and placentation in amniote vertebrates. Respir Physiol Neurobiol , 178, 39-50. PMID: 21470579 DOI.
Riquelme G. (2011). Review: Placental syncytiotrophoblast membranes--domains, subdomains and microdomains. Placenta , 32 Suppl 2, S196-202. PMID: 21272934 DOI.
Cartwright JE, Fraser R, Leslie K, Wallace AE & James JL. (2010). Remodelling at the maternal-fetal interface: relevance to human pregnancy disorders. Reproduction , 140, 803-13. PMID: 20837731 DOI.
Huppertz B. (2008). The anatomy of the normal placenta. J. Clin. Pathol. , 61, 1296-302. PMID: 18755720 DOI.
Wang Y, Zhao S. Vascular Biology of the Placenta. San Rafael (CA): Morgan & Claypool Life Sciences; 2010. Bookshelf NBK53247
Articles
Dhakal P, Kelleher AM, Behura SK & Spencer TE. (2020). Sexually dimorphic effects of forkhead box a2 (FOXA2) and uterine glands on decidualization and fetoplacental development. Proc. Natl. Acad. Sci. U.S.A. , , . PMID: 32900950 DOI.
Porto L, Aviram A, Jackson R, Carson M, Melamed N, Barrett J & Mei-Dan E. (2020). Lateral placentation and adverse perinatal outcomes. Placenta , 101, 1-3. PMID: 32905973 DOI.
Salafia CM, Yampolsky M, Misra DP, Shlakhter O, Haas D, Eucker B & Thorp J. (2010). Placental surface shape, function, and effects of maternal and fetal vascular pathology. Placenta , 31, 958-62. PMID: 20933281 DOI.
Yetter JF. (1998). Examination of the placenta. Am Fam Physician , 57, 1045-54. PMID: 9518951
Books
- Wang Y, Zhao S. Vascular Biology of the Placenta. San Rafael (CA): Morgan & Claypool Life Sciences; 2010. Available from: http://www.ncbi.nlm.nih.gov/books/NBK53247
- Boyd, J.D., Hamilton, W.J. 1970. The utero-placental circulatory system. In: The Human Placenta. W Heffer and Sons Ltd, London.
Historic Textbooks and Research
- Bloxam W. On the structure of the human placenta, and its connexion with the uterus. (1840)
- Herzog MA. A contribution to our knowledge of the earliest known stages of placentation and embryonic development in man. (1909) Amer. J Anat., 9(3): 361-400.
- Grosser O. VII. The development of the egg membranes and the placenta; menstruation in Keibel F. and Mall FP. Manual of Human Embryology I. (1910) J. B. Lippincott Company, Philadelphia.
- Bremer JL. The interrelations of the mesonephros, kidney and placenta in different classes of animals. (1918) Amer. J Anat. 19(2): 179-209.
- Fujimura G. Cytological studies on the internal secretory functions in the human placenta and decidua. (1921) J Morphol. 35(3): 486-576.
- Corner GW. Cyclic changes in the ovaries and uterus of swine, and their relations to the mechanism of implantation. (1921) Contrib. Embryol., Carnegie Inst. Wash. Publ. 394, :117-146.
- Dawson AB. The origin and occurrence of the single umbilical artery in normal and abnormal human fetuses. (1922) Anat. Rec. 24(5): 321-342.
- Boyd JD. Hamilton WJ. Electron microscopic observations on the cytotrophoblast contribution to the syncytium in the human placenta. (1966) J. Anat., 100(Pt 3): 535-48. PMID 5965440
- Strachan GI. The development and structure of the human placenta. (1923) J Obstet. and Gynaecol. (1923)
- Wislocki GE. and Bennett SB. The histology and cytology of the human and monkey placenta, with special reference to the trophoblast. (1943) Amer. J Anat. 337-448.
- Baker BL. Hook SJ. and Severinghaus AE. The cytological structure of the human chorionic villus and decidua parietalis. (1944) Amer. J Anat. 73(3): 291-325.
- Hertig AT. lnvolution of tissues in fetal life: a review. (1946) Anat. Rec. 94: 96-116.
- Ramsey EM. Corner GW. Jr. Donner MW. and Stran HM. Radioangiographic studies of circulation in the maternal placenta of the rhesus monkey: preliminary report. (1960) Proc. Natl. Acad. Sci. U.S.A., 46(7): 1003-8 PMID 16590693
- Ramsey EM. Placental Circulation. (1972) MCV Quarterly, 8(1): 61-68.
Search PubMed
Search April 2010
- Placenta Development - All (10032) Review (1896) Free Full Text (2435)
- Placental Development - All (9103) Review (1762) Free Full Text (2219)
- Placental Membranes - All (10083) Review (748) Free Full Text (1728)
Search Pubmed: Placenta Development | Placental Development | Placental Membranes
Additional Images
see all online Placental materials
Placental imaging PMID 29377190
Placental villi (EM) PMID 29377190
Placenta MRI 22 and 32 week
Placenta human and guinea-pig cartoon
Fetal membrane and placenta cartoon
Placenta spiral artery conversion
Uterine and placental vasculature
Placental cord cross-section
Human placenta viewed from the fetal side
Cord with one artery and one vein
Historic
| Historic Disclaimer - information about historic embryology pages
|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers)
|
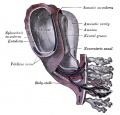
Keith 1902 Fig. 189. Diagram of the Remnants of the Umbilical Vein in the Adult
| Gray 1918
|
Gray H. Anatomy of the human body. (1918) Philadelphia: Lea & Febiger.
Historic drawing of early implantation (stage 8-9)
Fetal circulation overview
|
Terms
| Placenta Terms (expand to view)
|
- after-birth - term used to describe the delivery of placenta and placental membranes following birth of the child.
- allantois - An extraembryonic membrane, endoderm in origin extension from the early hindgut, then cloaca into the connecting stalk of placental animals, connected to the superior end of developing bladder. In reptiles and birds, acts as a reservoir for wastes and mediates gas exchange. In mammals is associated/incorporated with connecting stalk/placental cord fetal-maternal interface.
- amniocentesis - Clinical term for a prenatal diagnostic test where an ultrasound guided needle is used to extract a sample of the amniotic fluid. Amniocentesis
- anastomosis - Term used to describe the connection between two tubes. Applied to describe the connection between peripheral blood vessels without an intervening capillary bed.
- anchoring villi - (stem villi) describes the placental villi (embryonic) that attach to the decidua (maternal) tissue. The tip of the villi consists of a column of trophoblast cells attached to an epithelial plaque.
- angioblasts form clusters or blood islands on surface of yolk sac.
- angiogenesis - Term describing the development of new vessels from already existing vessels, this process is secondary to vasculogenesis which is the initial formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm).
- capsularis - portion of maternal decidua that covers the conceptus facing towards the uterine cavity.
- cerebroplacental ratio - (CPR) a doppler ultrasound measurement calculated as the simple ratio between the middle cerebral artery pulsatility index (MCA‐PI) and the umbilical artery pulsatility index (UA‐PI). Fetuses with an abnormal ratio are thought to be a predictor of adverse pregnancy outcome.
- chorioamnionitis - (CA) An intraamniotic puerperal infection described as having 3 forms: histologic, clinical (clinical chorioamnionitis, IAI), and subclinical. Intraamniotic infection is a common (2-4%) event in labor and the systemic inflammatory response can also lead to preterm birth and neonatal complications.
- chorion - The extraembryonic membrane generated from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange.
- chorionic cavity - The fluid-filled extraembryonic coelom (cavity) formed initially from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange. In humans, this cavity is lost during week 8 when the amniotic cavity expands and fuses with the chorion.
- chorion frondosum - (frondosum = leafy) The chorion found on conceptus oriented towards maternal blood supply where the majority of villi form and proliferate, will contribute the fetal component of the future placenta.
- chorion laeve - (laeve = smooth) The smooth chorion found on conceptus away from maternal blood supply (towards uterine epithelium and cavity) with very few villi present.
- chorionic somatomammotropin - (CSH, human lactogen) A hormone synthesized within the placenta by syncytiotrophoblast cells. This protein hormone (190 amino acid) has a structure is similar to pituitary growth hormone.
- chorionic villus sampling - (CVS) The taking a biopsy of the placenta, usually at the end of the second month of pregnancy, to test the fetus for genetic abnormalities.
- coelocentesis - A sampling of extracoelomic fluid usually for an early prenatal diagnostic technique.
- connecting stalk - the original extra-embryonic mesoderm structure attaching the embryonic disc to the chorion. The placental blood vessels form within this structure.
- cord blood - (human umbilical cord blood, HUCB) A term used to describe blood collected from the placenta usually after birth. Has been identified as a source of stem cells with potential therapeutic uses and is stored in Cord Blood Banks throughout the world.
- cord knotting Term describing umbilical or placental cord knotting. This occurs in about 1% prevents the passage of placental blood, pseudoknots also occur usually with no effect.
- cord presentation - A term used to describe at birth the presence of the umbilical cord between the fetal presenting part and the cervix, with or without membrane rupture.
- cord prolapse - A term used to describe at birth the descent of the umbilical cord through the cervix alongside (occult) or past (overt) the presenting part in the presence of ruptured membranes (incidence of 0.1% to 0.6%).
- cotyledon - (Greek, kotyle = a deep cup) In the embryos of seed plants, the "seed leaves," in which nutrients are stored for use after germination. In placental animals, the term is also to describe the leaf-like structure of the placenta surface.
- cytotrophoblast - The "cellular" trophoblast layer surrounding (forming a "shell") the early implanting conceptus. Beginning at uterine adplantation, proliferation and fusion of these cells is thought to form a second outer trophoblast layer, the syncytiotrophoblast. The cytotrophoblast layer contributes to formation of the placental villi, the functional component of the fetal placenta.
- decidua basalis - The term given to the uterine endometrium at the site of implantation where signaling transforms the uterine stromal cells (fibroblast-like) into decidual cells. This forms the maternal component of the placenta, the decidualization process gradually spreads through the remainder of the uterus, forming the decidua parietalis.
- decidua basalis reaction - Term describing the maternal endometrial changes that occur initially at the site of, and following, blastocyst implantation. Seen as a deposition of glycogen, fibrin and proliferation of blood vessels. See also decidualization.
- decidua capsularis - The term given to the uterine endometrium which has been converted to decidua surrounding the conceptus on the smooth chorion side.
- decidua parietalis - The term given to the remainder of the uterine endometrium, away from the site of implantation, that gradually becomes comverted to decidua.
- decidual cell - The uterine stromal cells (fibroblast-like) that differentiate in response to both steroid hormones (progesterone) and embryonic signals. These cells then alter uterine environment to support further embryonic development as well as producing cytokines related to prolactin (PRL) and have an innate immune function.
- decidual reaction - maternal endometrial reaction invoked in order to block the rapid extension of the implanting syncytium.
- decidualization - (decidualisation, decidual reaction) The process by which uterine stromal cells differentiate in response to both steroid hormones and embryonic signals into large epitheliod decidual cells. This process is essential for the progress of implantation and establishing fetal-maternal communication.
- DHEA - (dehydroepiandrosterone, androstenolone) precursor of sex steroid hormones and is converted to testosterone and estradiol. Postnatally, an abundant circulating steroid produced in the adrenal gland. The fetal adrenal cortex produces dehydroepiandrosterone sulfate (DHEA-S) used by the placenta to produce estrogens. DHEA, androstenedione, and testosterone can be metabolized to epiandrosterone, and etiocholanolone. PMID 15635500
- fetal drug addiction - occurs when drugs used maternally cross the placental barrier and can establish neural/physiological addiction in the unborn fetus. drugs
- fetal erythroblastosis - (Haemolytic Disease of the Newborn) A clinical term describing an immune response between fetal and maternal blood groups; from fetus Rh+ / maternal Rh-. The leakage of blood from fetus, particularly at birth, causes maternal anti-Rh antibodies, which is then dangerous for a 2nd or future pregnancies.
- fetal intra-abdominal umbilical vein varix - (FIUV, umbilical vein varix) focal dilatation of the umbilical venous diameter at the level of cord insertion, the dilatation diameter increases linearly with gestational age. Represent about 4% of umbilical cord abnormalities
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices.PMID 24883288
- fibrinoid layer - (Nitabuch's layer) A layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- floating chorionic villi - Term used to describe the placental microanatomy structure of chorionic villi that are not attached to the maternal decidua and float in the maternal blood-filled space (lacunae). Structurally the same as anchoring chorionic villi conceptus side that are attached to the maternal decidua.These villi go through the same stages of development: primary villi - secondary villi - tertiary villi
- hemotrophic nutrition - Term used to describe in late placenta development the transfer of blood-borne nutrition from maternal to embryo/fetuscompared to early histiotrophic nutrition.
- heterotopic pregnancy - (Greek, heteros = other) Clinical term for a very rare pregnancy of two or more embryos, consisting of both a uterine cavity embryo implantation and an ectopic implantation.
- histiotrophic nutrition - Term used to describe in early placenta development the intital transfer of nutrition from maternal to embryo (histiotrophic nutrition) compared to later blood-borne nutrition (hemotrophic nutrition). Histotroph is the nutritional material accumulated in spaces between the maternal and fetal tissues, derived from the maternal endometrium and the uterine glands. This nutritional material is absorbed by phagocytosis initially by blastocyst trophectoderm and then by trophoblast of the placenta. in later placental development nutrition is by the exchange of blood-borne materials between the maternal and fetal circulations, hemotrophic nutrition.
- Hofbauer cells - Cells found within placental villi connective tissue. Have a role as macrophages of mesenchymal origin with potentially additional functions (remodeling, vasculogenesis, regulation of stromal water content).
- Human chorionic corticotropin - (hCACTH) placental derived hormone equivilant to corticotropin (ACTH) from the pituitary.
- Human chorionic gonadotrophin - (hCG) like leutenizing hormone, supports corpus luteum, originally secreted by trophoblast cells.
- Human chorionic somatommotropin - (hCS, placental lactogen) hormone level increases in maternal blood through pregnancy, decreases maternal insulin sensitivity (raising maternal blood glucose levels and decreasing maternal glucose utilization) aiding fetal nutrition.
- Template:Hydatiform mole - A uterine tumour with "grape-like" placenta appearance without enclosed embryo formation, arises mainly from a haploid sperm fertilizing an egg without a female pronucleus. It is one form of gestational trophoblastic disease(GTD), a number of abnormalities including hydatiform mole, invasive mole, choriocarcinoma and placental site trophoblastic tumor (PSTT).
- hysterectomy – clinical term for the surgical removal of the uterus.
- Langhans layer - cytotrophoblast cell layer.
- maternal antibodies - antibodies from the mother's immune system that are capable of crossing placental barrier. They can provide immune protection to the embryo, but may also participate in immune disease (fetal erythroblastosis).
- maternal sinusoids - placental spaces around chorionic villi that are filled with maternal blood. This is the closest maternal/fetal exchange site.
- Nitabuch's layer - (fibrinoid layer) The layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- Morbidly adherent placenta (MAP) A general clinical term used to describe the different forms of abnormal placental implantation (Accreta, Increta and Percreta).
- oligohydramnios - Clinical term for the accumulation a deficiency of amniotic fluid during pregnancy. See also polyhydramnios, an excess of amniotic fluid.
- persistent right umbilical vein - (PRUV) A placental cord abnormality associated with fetal abnormalities and poor neonatal prognosis. The estimated incidence of persistent right umbilical vein in a low-risk population is 1 : 526. PMID 12047534
- polyhydramnios - Clinical term for the accumulation of excess amniotic fluid during pregnancy. See also oligohydramnios, a deficiency of amniotic fluid.
- placenta - (Greek, plakuos = flat cake) The developmental organ formed from maternal and fetal contributions in animals with placental development. In human, the placenta at term is a discoid shape "flat cake" shape; 20 cm diameter, 3 cm thick and weighs 500-600 gm. Placenta are classified by the number of layers between maternal and fetal blood (Haemochorial, Endotheliochorial and Epitheliochorial) and shape (Discoid, Zonary, Cotyledenary and Diffuse). The placenta has many different functions including metabolism, transport and endocrine.
- placenta accreta - The abnormal placental adherence, either in whole or in part of the placenta with absence of decidua basalis, leading to retention as an after-birth to the underlying uterine wall. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
- placental arteries - (umbilical arteries) In placental animals, the blood vessels which develop within the placental cord carrying relatively deoxygenated blood from the embryo/fetus to the placenta. In humans, there are two placental arteries continuous with the paired internal iliac arteries (hypogastric arteries) arising off the dorsal aortas. At birth this vessel regresses and form the remnant medial umbilical ligament.
- placental cord - (umbilical cord) The placental cord is the structure connecting the embryo/fetus to the placenta. It is initially extra-embryonic mesoderm forming the connecting stalk within which the placental blood vessels (arteries and veins) form. In human placental cords the placental blood vessels are initially paired, later in development only a single placental vein remains with a pair of placental arteries. This structure also contains the allantois, an extension from the hindgut cloaca then urogenital sinus. Blood collected from the placental cord following delivery is a source of cord blood stem cells.)
- placental diameter - is measured in the transverse section by calculating the maximum dimensions of the chorionic surface.
- placental growth factor - (PlGF) A growth factor of the vascular endothelial growth factor (VEGF) family, released from the placental trophoblast cells and other sources that stimulates blood vessel growth.
- placental malaria - The malarial infection of the placenta by sequestration of the infected red blood cells. This condition can be common in regions where malaria is endemic with women carrying their first pregnancy (primigravida).
- placenta membranacea - rare placental abnormality characterized by the presence of chorionic villi directly attached to and covering the fetal membranes. Placenta Membranacea
- placenta previa - placenta overlies internal os of uterus, abnormal bleeding, may require cesarian delivery.
- placental thickness - is measured at its mid-portion from the chorionic plate to the basilar plate, on a longitudinal plane (less than 4 cm at term). Excludes any abnormalities (fibroids, myometrial contractions, or venous lakes). The placental thickness approximates in millimeters to the weeks of gestation.
- placental vein - (umbilical vein) In placental animals, the blood vessels which develop within the placental cord carrying relatively oxygenated blood from the placenta to the embryo/fetus. In humans, there are initially two placental veins which fuse to form a single vein. The resence of paired veins in the placental cord can be indicative of developmental abnormalities.
- placentophagia - Term used to descrbe the maternal ingestion of afterbirth materials (placental membranes and amniotic fluid) that can occur following mammalian parturition (birth).
- primary villi - (primary chorionic villi) Term describing the earliest stage of embryonic placenta development. In humans, the conceptus during week 2 this first stage of chorionic villi development consists of only the trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) forming finger-like extensions into maternal decidua. Initially these finger-like projections cover the entire surface of chorionic sac and later become restricted to the placental surface. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development.
- pre-eclampsia - During pregnancy a combination of high blood pressure, protein in urine and fluid retention resulting in maternal sudden excessive swelling of the face, hands and feet. Eclampsia is the subsequent development of convulsions, kidney failure, liver failure, clotting problems or mortality.
- Rh alloimmunization - feto-maternal haemorrhage generally in late pregnancy results in an Rh-negative woman becoming sensitised to Rh-positive fetal cells that enter her circulation. Clinically treated with anti-D immune globulin prophylaxis, alloimmunization occurs in 9–10% of at-risk pregnancies. immune
- secondary villi - (secondary chorionic villi) Term describing the second stage of embryonic placenta development. In humans, the conceptus during week 3 onward this stage of chorionic villi development consists of the trophoblastic shell cells (syncytiotrophoblast and cytotrophoblasts) filled with extraembryonic mesoderm forming finger-like extensions into maternal decidua. Initially these finger-like projections cover the entire surface of chorionic sac and later become restricted to the placental surface. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development. Placental villi stages: primary villi - secondary villi - tertiary villi
- syncytiotrophoblast - A multinucleated cell currently thought to form by the fusion of another trophoblast cell the cytotrophoblasts, within the trophoblast layer (shell) of the implanting conceptus. In early development, these cells mediate implantation of the conceptus into the uterine wall and secrete the hormone (Template:Human Chorionic Gonadotrophin, hCG) responsible for feedback maintainance of the corpus luteum (in maternal ovary) and therefore maintaining early pregnancy.
- trophoblast - (trophectoderm, Greek, trophe = "nutrition" and blast = a primordial cell) cells that firstly support adplantation, implantation and endocrine support of pregnancy. Contribute to the extraembryonic tissues, fetal placenta and membranes. Initially form 2 populations individual cytotrophoblast cells and their fused multinucleate syncytiotrophoblast cells.
- Twin-twin transfusion syndrome - (TTTS) in monozygotic twins with monochorionic and diamniotic placenta, with intrauterine blood transfusion from one twin (donor) to another twin (recipient) where there is an imbalance of blood flow from the donor twin to the recipient twin. Clinically diagnosed by the alternate presence of polyhydramnios in one fetus and oligohydramnios in the co-twin, occurs in about 10% of monochorionic twins.
- umbilical cord (placental cord) fetal attachment cord 1-2 cm diameter, 30-90cm long, covered with amniotic attached to chorionic plate, umbilical vessels (artery, vein) branch into chorionic vessels. Vessels anastomose within the placenta.
- umbilical vein varix - (fetal intra-abdominal umbilical vein varix, FIUV) focal dilatation of the umbilical venous diameter at the level of cord insertion, the dilatation diameter increases linearly with gestational age. Represent about 4% of umbilical cord abnormalities
with an incidence of about 2.8 per 1,000 pregnancies, there is also a rarer form of extra-abdominal varices. PMID 24883288
- vasculogenesis - formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm) followed by angiogenesis which is the development of new vessels from already existing vessels.
- vasculosyncytial membranes - localised areas of the placental villous membrane where the barrier thickness separating maternal and fetal circulations is reduced to as little as 1-2 microns. PMID 1287078
- villi - Plural of villus, which is a thin projection from a surface. The term in development is used to describe the individual functional units together of the fetal placenta.
- virus - small infectious agents that may cross the placental barrier. Can infect embryo and/or placenta and cause developmental abnormalities. (e.g. cytomegalovirus, rubella, measles).
- Wharton's jelly - placental cord (umbilical cord) gelatinous connective tissue composed of myofibroblast-like stromal cells, collagen fibers, and proteoglycans. Increases in volume (myxomatous, connective tissue embedded in mucus) at parturition (birth) to assist closure of placental blood vessels. Matrix cells from Wharton's jelly have recently been identified as a potential source of mesenchymal stem cells (MSC), also called mesenchymal stromal cell. This placental cord substance is named after Thomas Wharton (1614-1673) an English physician and anatomist who first described this placental tissue.
|
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- The Human Placenta Project - a collaborative research effort, launched by the NICHD to understand the role of the placenta in health and disease.Human Placenta Project | Video
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 27) Embryology Placenta Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Placenta_Development
- What Links Here?
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G