Endocrine System Development
| Embryology - 25 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
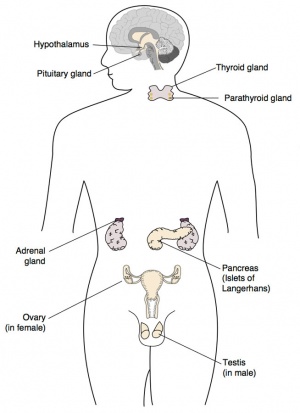
The endocrine system resides within specific endocrine organs and both organs and tissues with other specific functions. Epithelia (ectoderm and endoderm) form the majority of the “ductless” endocrine glands like gastrointestinal and skin associated “ducted” glands. Differentiation of several also organs involves a epithelial/mesenchye interaction, seen in repeated in many differentiation of many different tissues. The endocrine glands produce hormones, which are distributed by the vascular system to the many body tissues, subsequently these organs are richly vascularized.
Hormones are recognised by either cell surface receptors (modified amino acids, peptides, proteins) or cytoplasmic/nuclear receptors (steroids). Hormones “orchestrate” responses in other tissues, including other endocrine organs, and these overall effects can be similar or different in different tissues. In addition, these hormone effects (like music) can be rapid, slow, brief, diurnal, or long-term. Hormone effects can be mimicked, stimulated, and blocked by therapeutic drugs, nutritional and environmental chemicals.
The human fetus is dependent upon endocrine development for hormones, which support normal development. Peripheral endocrine glands (thyroid, pancreas, adrenals, gonads) form early in the second month from epithelial/mesenchye interactions and differentiate into the third month. The fetus also has a unique hormonal system that combines not only its own developing endocrine system, but also that of the corpus luteum, placenta and maternal hormones.
Abnormal endocrine development/function can impact on many different systems. For example, insufficient maternal dietary iodine impacts on fetal thyroid gland thyroid hormone production, which in turn can lead to abnormal neural development. Alternatively, we now know many environmental and therapeutic chemicals have a wide range of effects on the endocrine system.
Sex hormones from the gonads have significant effects prenatally and postnatally, specifically at puberty with a role to play in male/female biological maturity and have wide actions throughout the body.
This current page provides a general introduction to the endocrine system, use the links below to explore development of specific endocrine organs.
Pineal |
Hypothalamus |
Pituitary |
Thyroid |
Thymus |
Pancreas |
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References See also specific endocrine organ pages for more specific search options. Search term: Endocrine Development | Endocrine Embryology
|
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Textbooks
In general, not dealt with as a system in many embryology textbooks, so various chapters: nervous system, head, gastrointestinal tract, reproductive organs, etc. See the online Endocrinology textbook for better descriptions of these tissues.
|
|
- Human Embryology (3rd ed.) Larson Chapter 9 Gastrointestinal, Chapter 10 Gonad, Kidney Chapter 12 Head
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapters 10: p230-233; Ch12: p280-282; Ch13: p319-347
- Lectures - Lecture - Endocrine Development | 2010 | 2009 |
- The Endocrine System - An Overview (PDF)
| Larsen's Human Embryology - UNSW Students |
|---|
Schoenwolf, G.C., Bleyl, S.B., Brauer, P.R., Francis-West, P.H. & Philippa H. (2015). Larsen's human embryology (5th ed.). New York; Edinburgh: Churchill Livingstone. UNSW students have full access to this textbook edition through UNSW Library subscription (with student Zpass log-in).
|
| Endocrine Links: Introduction | BGD Lecture | Science Lecture | Lecture Movie | pineal | hypothalamus | pituitary | thyroid | parathyroid | thymus | pancreas | adrenal | endocrine gonad | endocrine placenta | other tissues | Stage 22 | endocrine abnormalities | Hormones | Category:Endocrine | ||
|
Objectives
- Understand the main steps in the development of the thyroid, parathyroid, adrenal, pituitary, pineal glands, thymus and gonads.
- Have a general understanding of the chief functions of these endocrine organs.
- Understand the endocrine contribution to embryo development.
- Understand the endocrine role of the placenta during development.
- Have a general understanding of different types of hormones and their signaling actions.
Hormones

Hormone Types
- Amino acid derivatives - noradrenaline (norepinepherine), adrenalin (epinepherine) , thyroid hormone
- Proteins, peptides - thyroid stimulating hormone, leutenising hormone, follicle stimulating hormone
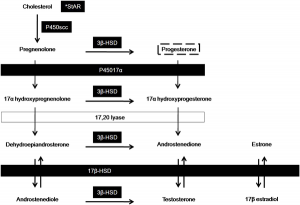
- Steroids - androgens, glucocorticoids, mineralocorticoids
Hormone Actions
- Autocrine - acts on self (extracellular fluid)
- Paracrine - acts locally (extracellular fluid)
- Endocrine - acts by secretion into blood stream (endocrine organs are richly vascularized)
Hormone Receptors
Hormones are recognised by either cell surface receptors (modified amino acids, peptides, proteins) or cytoplasmic/nuclear receptors (steroids).
| Interested in endocrine and hormone history? Listen to ABC Radio Ockham's Razor 2005-07-31 Centenary of the word "hormone" (File:Audio - centenary of hormone.mp3), by Sydney medical scientist (from SOMS) and writer Dr John Carmody commemorates the centenary of the entry of the word 'hormone' into the English language. |
- Links: Hormones
Endocrine Origins
- Derived from epithelia - covering embryo, lining gastrointestinal tract, lining coelomic cavity (mesothelium)
- Also mesenchymal contribution
Development Overview
See specific endocrine organ development.
| Human Endocrine - Embryonic Timeline |
|---|
| Data based on data from O'Rahilly (1983).[4] |
Stage 13 (week 4)
|
Stage 14 (week 5)
|
Stage 15
|
Stage 16 (week 6)
|
Stage 17
|
Stage 18 (week 7)
|
Stage 19
|
Stage 20 (week 8)
(1938), of migration of and covering by "cells derived from the cervical sinus".
Weller (1933, Fig. 23) showed parathyroid 3 still rostral to parathyroid 4 at 23 mm, whereas (presumably due to variation in the "descent" of the thymus) (Norris 1937, Fig. 4[20]) showed parathyroid 3 rostral to, level with, and caudal to parathyroid 4 in embryos of 16-17 mm. |
Stage 21
|
Stage 22
|
Stage 23
|
- Links: Endocrine embryo table
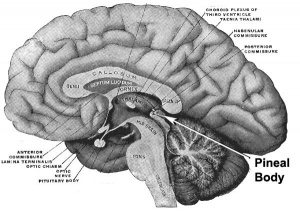
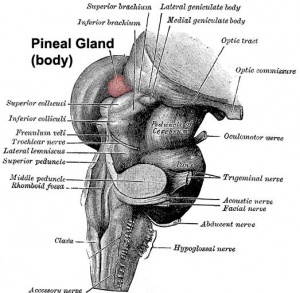
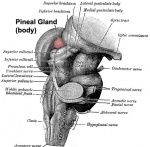
Pineal Gland
- part of epithalmus - neurons, glia and pinealocytes
- pinealocytes secrete melatonin - cyclic nature of activity, melatonin lowest during daylight
- inhibit hypothalamic secretion of GnRH until puberty, pineal gland then rapidly regresses.
- other activities - possibly gamete maturation, antioxidant effect, protect neurons?
Pineal Development
- Neuroectoderm - prosenecephalon then diencephalon
- caudal roof, median diverticulum, epiphysis
- Initially a hollow diverticulum, cell proliferation to solid, pinealocytes (neuroglia), cone-shaped gland innervated by epithalmus
Hypothalamus
Hormones - Thyrotrophin releasing hormone (TRH), Corticotrophin releasing hormone (CRH), Arginine vasopressin (AVP), Gonadotrophin releasing hormone (GnRH), Growth hormone releasing hormone (GHRH), Somatostatin, Prolactin relasing factor (PRF), Dopamine
Hypothalamus Development
- Neuroectoderm - prosenecephalon then diencephalon
- ventro-lateral wall intermediate zone proliferation
- Mamillary bodies - form pea-sized swellings ventral wall of hypothalamus
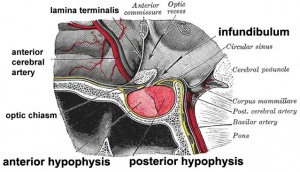
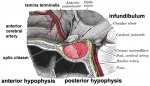
Pituitary
Anterior pituitary hormones - Thyroid-stimulating hormone (TSH), Adrenocorticotrophic hormone (ACTH), Luteinizing hormone (LH), Follicle-stimulating hormone (FSH), Somatotrophin/growth hormone (GH), Prolactin (PRL), Melanocyte-stimulating hormone (MSH)
Posterior pituitary hormones - Oxytocin, Arginine vasopressin
Pituitary Development
|
Blue - neural tube ectoderm
Red - surface ectoderm |
- Dual ectoderm origins
- Ectoderm - ectoderm roof of stomodeum, Rathke's pouch, adenohypophysis
- Neuroectoderm - prosenecephalon then diencephalon, neurohypophysis
Adenohypophysis
- Anterior wall proliferates - pars distalis
- Posterior wall little growth – pars intermedia
- Rostral growth around infundibular stem – pars tuberalis
Neurohypophysis
- Infundibulum – median eminence, infundibulum, pars nervosa
Pituitary Timeline
- Week 4 - hypophysial pouch, Rathke’s pouch, diverticulum from roof
- Week 5 - elongation, contacts infundibulum, diverticulum of diencephalon
- Week 6 - connecting stalk between pouch and oral cavity degenerates
- Week 10 - growth hormone and ACTH detectable
- Week 16 - adenohypophysis fully differentiated
- Week 20 to 24 - growth hormone levels peak, then decline
Links: Endocrine - Pituitary Development | Embryo Images - Pituitary
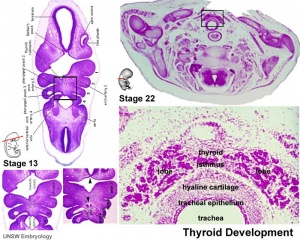
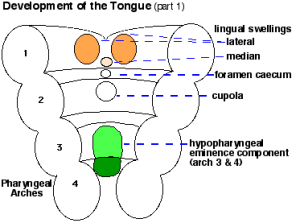
Thyroid
- Functions from wk10, required for neural development, stimulates metabolism (protein, carbohydrate, lipid), reduced/absence = cretinism (see abnormalities)
Hormones - (amino acid derivatives) Thyroxine (T4), Triiodothyronine (T3)
Thyroid Development
- thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- tongue grows, cells descend in neck
- thyroglossal duct - proximal end at the foramen cecum of tongue thyroglossal duct
- thyroid diverticulum - hollow then solid, right and left lobes, central isthmus
Thyroid Timeline
- 24 days - thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- Week 11 - colloid appearance in thyroid follicles, iodine and thyroid hormone (TH) synthesis
growth factors (insulin-like, epidermal) stimulates follicular growth
Fetal Thyroid Hormone
- Initial secreted biologically inactivated by modification, late fetal secretion develops brown fat
- Iodine deficiency- during this period, leads to neurological defects (cretinism)
- Birth - TSH levels increase, thyroxine (T3) and T4 levels increase to 24 h, then 5-7 days postnatal decline to normal levels
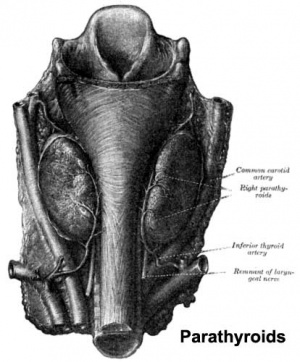
Parathyroid
- Parathyroid Hormone - Increase calcium ions [Ca2+], stimulates osteoclasts, increase Ca GIT absorption (opposite effect to calcitonin)
- Adult Calcium and Phosphate - Daily turnover in human with dietary intake of 1000 mg/day
- secreted by chief cells
Principal cells cords of cells
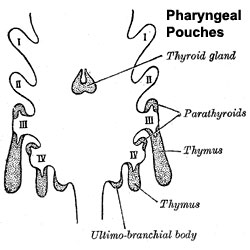
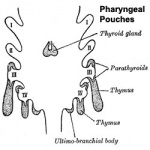
Parathyroid Development
- Endoderm - third and fourth pharyngeal pouches, could also have ectoderm and neural crest
- 3rd Pharyngeal Pouch - inferior parathyroid, initially descends with thymus
- 4th Pharyngeal Pouch - superior parathyroid
- Week 6 - diverticulum elongate, hollow then solid, dorsal cell proliferation
- Fetal parathyroids - respond to calcium levels, fetal calcium levels higher than maternal
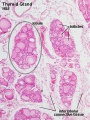
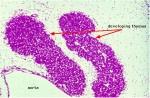
Thymus
- Thymus - bone-marrow lymphocyte precursors become thymocytes, and subsequently mature into T lymphocytes (T cells)
- Thymus hormones - thymosins stimulate the development and differentiation of T lymphocytes
Thymus Development
- Endoderm - third pharyngeal pouch
- Week 6 - diverticulum elongates, hollow then solid, ventral cell proliferation
- Thymic primordia - surrounded by neural crest mesenchyme, epithelia/mesenchyme interaction
- Note in contrast to this historic image (shown here), current research has shown that the human thymic epithelium derives solely from the third pharyngeal pouch (as in the mouse). [23]
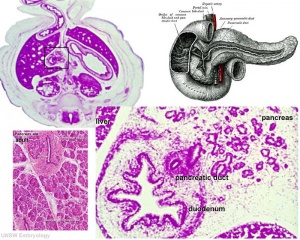
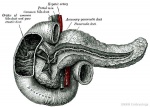
Pancreas
- Functions - exocrine (amylase, alpha-fetoprotein), 99% by volume; endocrine (pancreatic islets) 1% by volume
- Exocrine function - begins after birth
- Endocrine function - from 10 to 15 weeks onward hormone release
- exact roles of hormones in regulating fetal growth?
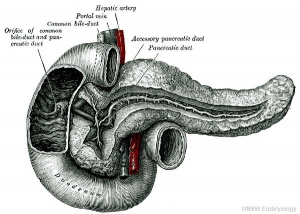
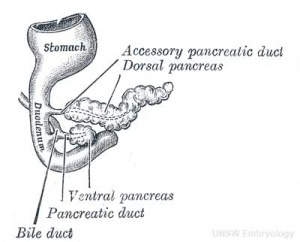
Pancreas Development
- Pancreatic buds - duodenal level endoderm, splanchnic mesoderm forms dorsal and ventral mesentery, dorsal bud (larger, first), ventral bud (smaller, later)
- Pancreas Endoderm - pancreas may be opposite of liver
- Heart cells promote/notochord prevents liver formation
- Notochord may promote pancreas formation
- Heart may block pancreas formation
- Duodenum growth/rotation - brings ventral and dorsal buds together, fusion of buds
- Pancreatic duct - ventral bud duct and distal part of dorsal bud, exocrine function
- Islet cells - cords of endodermal cells form ducts, from which cells bud off to form islets
Pancreatic Islets
- Islets of Langerhans - 4 endocrine cell types
- Alpha - glucagon, mobilizes lipid
- Beta - insulin, increase glucose uptake
- Beta cells, stimulate fetal growth, continue to proliferate to postnatal, in infancy most abundant
- Delta - somatostatin, inhibits glucagon, insulin secretion
- F-cells - pancreatic polypeptide
Pancreas Timeline
- Week 7 to 20 - pancreatic hormones secretion increases, small amount maternal insulin
- Week 10 - glucagon (alpha) differentiate first, somatostatin (delta), insulin (beta) cells differentiate, insulin secretion begins
- Week 15 - glucagon detectable in fetal plasma
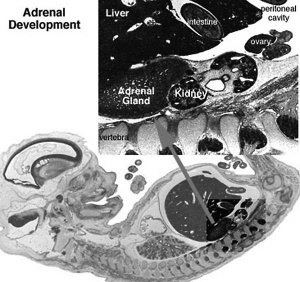
Adrenal
- Richly vascularized - arterioles passing through cortex, capillaries from cortex to medulla, portal-like circulation
- Fetal Cortex - produces a steroid precursor (DEA), converted by placenta into estrogen
- Adult Medulla - produces adrenalin (epinephrine), noradrenaline (norepinephrine)
- Fetal adrenal hormones - influence lung maturation
Adrenal cortical hormones - (steroids) Cortisol, Aldosterone, Dehydroepiandrosterone
- zona glomerulosa - regulated by renin-angiotensin-aldosterone system controlled by the juxtaglomerular apparatus of the kidney.
- zona fasciculata - regulated by hypothalamo-pituitary axis with the release of CRH and ACTH respectively.
Adrenal medullary hormones - (amino acid derivatives) Epinephrine, Norepinephrine
Adrenal Development
- Fetal Adrenals - fetal cortex later replaced by adult cortex
- Week 6 - fetal cortex, from mesothelium adjacent to dorsal mesentery; Medulla, neural crest cells from adjacent sympathetic ganglia
- Adult cortex - mesothelium mesenchyme encloses fetal cortex
Adrenal Cortex
- Late Fetal Period - differentiates to form cortical zones
- Birth - zona glomerulosa, zona fasiculata present
- Year 3 - zona reticularis present
Endocrinology - Adrenal Cortex Development
Adrenal Medulla
- neural crest origin, migrate adjacent to coelomic cavity, initially uncapsulated and not surrounded by fetal cortex, cells have neuron-like morphology
- 2 cell types - secrete epinepherine (adrenaline) 80%; secrete norepinepherine (noradrenaline* 20%
Gonad
HPG Axis - Endocrinology - Simplified diagram of the actions of gonadotrophins
Gonad Development
- mesoderm - mesothelium and underlying mesenchyme, primordial germ cells
- Gonadal ridge - mesothelium thickening, medial mesonephros
- Primordial Germ cells - yolk sac, to mesentery of hindgut, to genital ridge of developing kidney
Differentiation
- testis-determining factor (TDF) from Y chromosome: presence (testes), absence (ovaries)
Testis
- 8 Weeks, mesenchyme, interstitial cells (of Leydig) secrete testosterone, androstenedione
- 8 to 12 Weeks - hCG stimulates testosterone production
- Sustentacular cells - produce anti-mullerian hormone to puberty
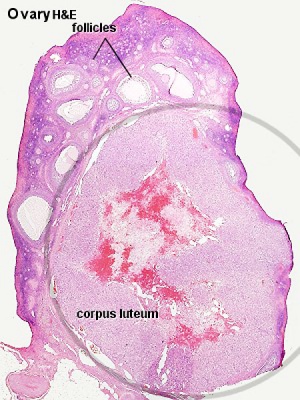
Ovary
- X chromosome genes regulate ovary development
Corpus Luteum
A maternal endocrine organ that develops within the ovary in all mammalian species from the ovulating follicle[24]. The key function of this endocrine organ is to maintain pregnancy in response to endocrine signals from the implanting conceptus (chorionic ganadotrophin). Corpus luteum steroidogenesis then alters the normal female reproductive cycle, maintains the endometrial lining of the uterus, and acts on the maternal endocrine system. The corpus luteum, depending upon the species, produces a range of androgens, estrogens and progesterone.
| Corpus Luteum Links: anatomy overview | image - histology overview | image - Layers granulosa and theca | image - Layers detail granulosa and theca | image - low power label | image - high power label | image - low power | image - high power | image - corpus albicans | theca and granulosa lutein cells | Granulosa cell | corpus luteum | granulosa lutein cells | theca lutein cells | corpus albicans | ovary | menstrual cycle |
| Historic Papers: 1969 corpus luteum ultrastructure 1 | 1969 corpus luteum ultrastructure 2 |
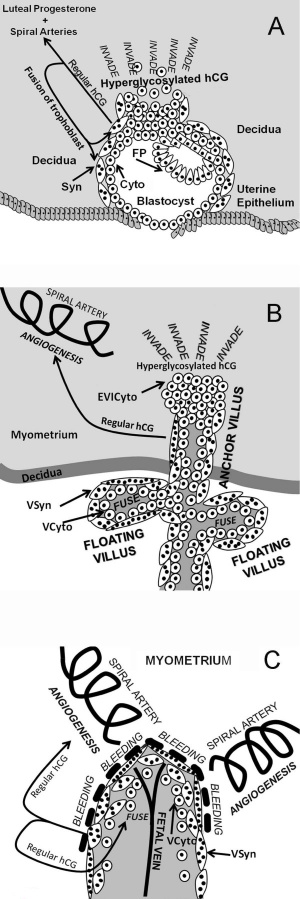
Placenta
- Human chorionic gonadotrophin (hCG) - like leutenizing hormone, supports corpus luteum in ovary, pregnant state rather than menstrual, maternal urine in some pregnancy testing
- Human chorionic somatommotropin (hCS) - or placental lactogen stimulate (maternal) mammary development
- Human chorionic thyrotropin (hCT)
- Human chorionic corticotropin (hCACTH)
- progesterone and estrogens - support maternal endometrium
- Progesterone-Associated Endometrial Protein (PAEP, pregnancy protein-14, PP14) - glycoprotein hormone from decidualized endometrium with possible immunoregulatory activities.
- Relaxin
- Placenta - Maternal (decidua) and Fetal (trophoblastic cells, extraembryonic mesoderm) components
- Endocrine function - maternal and fetal precursors, synthesis and secretion
- Protein Hormones - chorionic gonadotropin (hCG), chorionic somatomammotropin (hCS) or placental lactogen (hPL), chorionic thyrotropin (hCT), chorionic corticotropin (hCACTH)
- hCG - up to 20 weeks, fetal adrenal cortex growth and maintenance
- hCS – rise through pregnancy, stimulates maternal metabolic processes, breast growth
- Steroid Hormones - progesterone (maintains pregnancy), estrogens (fetal adrenal/placenta)
- Protein Hormones - chorionic gonadotropin (hCG), chorionic somatomammotropin (hCS) or placental lactogen (hPL), chorionic thyrotropin (hCT), chorionic corticotropin (hCACTH)
- Links: endocrine placenta
Other Endocrine
Endocrine Heart
- Atrial natriuretic peptide (ANP) - Increase Filtration rate / decrease Na+ reabsorption
- Endothelins - ET-1, ET-2, ET-3, Vasoconstriction / Increase NO
- Nitric oxide (NO) - Vasodilatation
Endocrine Kidney
- Renin - Increase Angiotensin-aldosterone system
- Prostaglandins - decrease Na+ reabsorption
- Erythropoietin - Increase Erythrocyte (rbc) production
- 1,25 (OH)2 vitamin D - calcium homeostasis
- Prekallikreins - Increase Kinin production
GIT Endocrine
Enteric control of digestive function
- Gastrin - Secreted from stomach (G cells), role in control of gastric acid secretion
- Cholecystokinin - small intestine hormone, stimulates secretion of pancreatic enzymes and bile
- Secretin - small intestine hormone (epithelial cells), stimulates secretion of bicarbonate-rich fluids from pancreas and liver
Adipose Tissue
- Leptin - polypeptide hormone produced in adipose and many other tissues with also many different roles
- Adiponectin - regulation of energy homeostasis and glucose and lipid metabolism, as well as acting as an anti-inflammatory on the cellular vascular wall
- Resistin - (for resistance to insulin, RETN) a 108 amino acid polypeptide and the related resistin-like protein-beta (Resistin-like molecule-beta, RELMbeta) stimulate endogenous glucose production
- Links: Endocrine - Other Tissues
Endocrine Functional Changes
- Puberty - Increased activity
- Menopause - Decreased activity
- Disease - (diabetes, thyroid, kidney) suggested trends that genetics, health, nutrition, lifestyle may influence time that these events occur
- Pharmaceutical impact - birth control, steroids, Hormone Replacement Therapy (HRT)
References
- ↑ Dames P, Puff R, Weise M, Parhofer KG, Göke B, Götz M, Graw J, Favor J & Lechner A. (2010). Relative roles of the different Pax6 domains for pancreatic alpha cell development. BMC Dev. Biol. , 10, 39. PMID: 20377917 DOI.
- ↑ Kelberman D, Rizzoti K, Lovell-Badge R, Robinson IC & Dattani MT. (2009). Genetic regulation of pituitary gland development in human and mouse. Endocr. Rev. , 30, 790-829. PMID: 19837867 DOI.
- ↑ <pubmed>17464358</pubmed>| PMC1853070 | Nucl Recept Signal.
- ↑ O'Rahilly R. The timing and sequence of events in the development of the human endocrine system during the embryonic period proper. (1983) Anat. Embryol., 166: 439-451. PMID 6869855
- ↑ O'Rahilly R. Developmental Stages in Human Embryos, Including a Survey of the Carnegie Collection. Part A: Embryos of the First Three Weeks (Stages 1 to 9). (1973) Carnegie Instn. Wash. Publ. 631. Washington, D.C.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Weller GL. Development of the thyroid, parathyroid and thymus glands in man. (1933) Contrib. Embryol., Carnegie Inst. Wash. 24: 93-139.
- ↑ 7.0 7.1 7.2 7.3 Norris EH. The morphogenesis and histogenesis of the thymus gland in man: in which the origin of the Hassal's corpuscles of the human thymus is discovered. (1938) Contrib Embryol Carneg Instn 27: 191-207.
- ↑ Politzer G. Zur Abgrenzung des Anlagebegriffes, er6rtert an der Friihentwicklung von Parathyreoidea, Pancreas und Thyreoidea (Delineation of the development of the parathyroids, the pancreas, and the thyroid gland). (1952) Acta Anat 15:68-84.
- ↑ 9.0 9.1 Streeter GL. Developmental horizons in human embryos. Description of age group XIII, embryos about 4 or 5 millimeters long, and age group XIV, period of indentation of the lens vesicle. (1945) Carnegie Instn. Wash. Publ. 557, Contrib. Embryol., Carnegie Inst. Wash., 31: 27-63.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 O'Rahilly R. The early development of the hypophysis cerebri in staged human embryos. (1973) Anat Rec 175:511.
- ↑ 11.0 11.1 Politzer G, Hann F. Uber die Emwicklung der branchiogenen Organe beim Menschen (On the development of the branchiogenic organs in humans). (1935) Z Anat Entw Gesctl 104: 671-708.
- ↑ 12.0 12.1 Blechschmidt E. Die prdnatalen Organsysteme des Menschen. (1973) Hippokrates, Stuttgart.
- ↑ 13.0 13.1 Streeter GL. Developmental horizons in human embryos. Description of age groups XV, XVI, XVII, and XVIII, being the third issue of a survey of the Carnegie collection. (1948) Contrib. Embryol., Carnegie Inst. Wash. 575, 32: 133-203.
- ↑ Odgers PN. Some observations on the development of the ventral pancreas in man. (1930) J. Anat., 65(1): 1-7. PMID 17104298
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 Crowder RE. The development of the adrenal gland in man, with special reference to origin and ultimate location of cell types and evidence in favor of the "cell migration" theory. (1957) Contrib. Embryol., Carnegie Inst. Wash. 36, 193-210.
- ↑ 16.0 16.1 16.2 16.3 16.4 Turketwitsch N. Die Entwicklung der Zirbeldrüse des Menschen (The development of the pineal gland in humans). (1933) Morphol Jb 72: 379-445.
- ↑ 17.0 17.1 17.2 17.3 O'Rahilly R. The development of the epiphysis cerebri and the subcommissural complex in staged human embryos. (1968) Anat. Rec., 160: 488-489.
- ↑ Grosser O. The development of the pharynx and of the organs of respiration. In: F. Keibel, F.P. Mall (ed) Manual of human embryology. (1912) Philadelphia, Lippincott, pp 446-497.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 Jirásek JE. Human fetal endocrines. (1980) Martinus Nijhoff Publishers BV, The Hague. Springer
- ↑ 20.0 20.1 20.2 Norris EH. The parathyroid glands and the lateral thyroid in man: their morphogenesis, histogenesis, topographic anatomy and prenatal growth. (1937) Contrib Embryol Carneg Instn 26: 247-294
- ↑ 21.0 21.1 <pubmed>5117462</pubmed>
- ↑ Siegler R. The thymus and the unicorn-two great myths of gross anatomy. (1969) Anat Rec. 163: 264.
- ↑ <pubmed>23571219</pubmed>
- ↑ <pubmed>17464358</pubmed>
Journals
Endocrine Development This series is devoted to specific areas of fetal, neonatal, pediatric and adolescent endocrinology. It addresses a wide range of relevant issues in the context of a well defined subject and covers new areas of clinical and basic research.
Textbooks

|
Endocrinology - An Integrated Approach Stephen Nussey and Saffron Whitehead, St. George's Hospital Medical School, London, UK Oxford: BIOS Scientific Publishers; 2001.
ISBN-10: 1-85996-252-1 Copyright © 2001, BIOS Scientific Publishers Limited. Bookshelf Link |

|
Endotext De Groot LJ, Beck-Peccoz P, Chrousos G, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Bookshelf Link |
Reviews
Özen S & Darcan Ş. (2011). Effects of environmental endocrine disruptors on pubertal development. J Clin Res Pediatr Endocrinol , 3, 1-6. PMID: 21448326 DOI.
Articles
Search PubMed
Search Pubmed: Endocrine Development
NCBI - Policies and Guidelines | PubMed | Help:Reference Tutorial
Additional Images
Embryonic Histology
Adult Histology
| Endocrine Terms | ||
|---|---|---|
| ||
|
| System Links: Introduction | Cardiovascular | Coelomic Cavity | Endocrine | Gastrointestinal Tract | Genital | Head | Immune | Integumentary | Musculoskeletal | Neural | Neural Crest | Placenta | Renal | Respiratory | Sensory | Birth |
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 25) Embryology Endocrine System Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Endocrine_System_Development
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G