Neonatal Diagnosis
| Embryology - 20 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose. |
Introduction
In the early 1950's Virginia Apgar published the research article that was the basis of a simple diagnostic test, the 10-point Apgar score, for neonatal well-being at birth that continues to be used today.
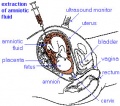
There are a number of different neonatal diagnosis or screening (newborn screening) programs in different countries testing for various "common" abnormalities and infections. In addition to the Guthrie test there are also physical tests for hip displasia and a growing number of countries testing of newborn hearing. There are also a range of simple clinical tests for postnatal neurological development.
The Neonatal period is considered the postnatal development categorised from birth to 1 month (4 weeks).
| Neonatal Diagnosis Links: neonatal diagnosis | Apgar test | Guthrie test | hearing test | Electrocardiogram (ECG/EKG) | X-ray | Tandem mass spectrometry | Classification of Diseases |
Diagnosis Categories
- Prenatal diagnosis - number of different techniques (non-invasive, invasive) for determining normal development
- Neonatal diagnosis (Apgar test, Guthrie test (heel-prick test), hearing test)
- Maternal diagnosis - often pregnancy will expose maternal health problems
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Newborn Screening <pubmed limit=5>Newborn Screening</pubmed> |
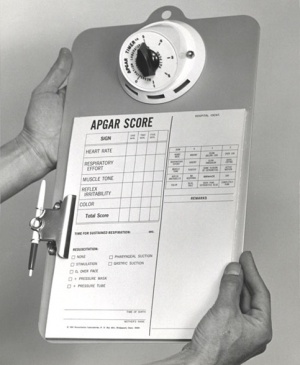
Apgar Test
A historic neonatal test designed by Dr Virginia Apgar[3] used in nearly all maternity clinics to assess the newborn infants well being assigned scores for each of 5 indicators: Heart Rate, Respiratory Effort, Reflex Irritability, Muscle Tone, Colour Measured at one and five minutes after birth the Score values are totalled for all indicators: 7-10 is considered normal, 4-7 may require resuscitative measures, 3 and below require immediate resuscitation. In recent years there has been some controversy of the relevance and accuracy of some of the criteria used in this test, though many feel it is still an invaluable initial assessment tool particularly where medical services are limited.
- Measured at one and five minutes after birth.
- The Score values are totalled for all indicators
- 7 to 10 is considered normal
- 4 to 7 may require resuscitative measures
- 3 and below require immediate resuscitation
| Indicator | Score 0 | Score 1 | Score 2 |
| Activity (muscle tone) |
Limp; no movement | Some flexion of arms and legs | Active motion |
| Pulse (heart rate) |
No heart rate | Fewer than 100 beats per minute | At least 100 beats per minute |
| Grimace (reflex response) |
No response to airways being suctioned | Grimace during suctioning | Grimace and pull away, cough, or sneeze during suctioning |
| Appearance (color) |
The baby's whole body is completely bluish-gray or pale | Good color in body with bluish hands or feet | Good color all over |
| Respiration (breathing) |
Not breathing | Weak cry; may sound like whimpering, slow or irregular breathing | Good, strong cry; normal rate and effort of breathing |
| Table data[3] Apgar test - Measured at one and five minutes after birth, the score values are totalled for all indicators: | |||
| Total Score: | 3 and below require immediate resuscitation | 4 to 7 may require resuscitative measures | 7 to 10 is considered normal |
|---|---|---|---|
- Links: Apgar test
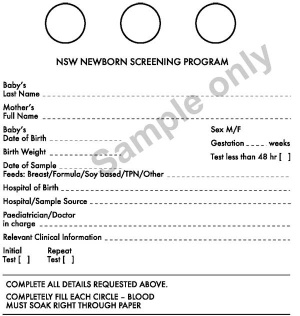
Guthrie Test
A blood screening test developed by Dr Robert Guthrie[4] (1916-95) at University of Buffalo. The test is carried out on neonatal (newborn) blood detecting markers for a variety of known disorders (phenylketonuria (PKU), hypothyroidism and cystic fibrosis). In NSW and Victoria, the Guthrie Cards are currently stored indefinitely.
Note - The specific type of disorders screened for by this test varies by state and country around the world.
- Links: Guthrie test
Screened Disorders
- Biotinidase Deficiency
- Congenital Adrenal Hyperplasia (CAH)
- Congenital Hypothyroidism (CH)
- Congenital Toxoplasmosis
- Cystic Fibrosis (CF)
- Galactosemia (GAL)
- Homocystinuria
- Maple Syrup Urine Disease (MSUD)
- Medium-Chain Acyl-CoA Dehydrogenase Deficiency (MCAD)
Biotinidase Deficiency
(multiple carboxylase deficiency) Defined by time of onset (early or late) and enzyme deficiency level (profound or partial).
- Early-onset multiple carboxylase deficiency is caused by mutation in the holocarboxylase synthetase gene.
- Late-onset multiple carboxylase deficiency with biotinidase deficiency is caused by mutation in the biotinidase gene.
Mean serum biotinidase enzyme activity/level compared to normal.
- profound- less than 10% of normal
- partial - 10% - 30% of normal
Characteristics include:
- neurologic abnormalities - seizures, hypotonia, ataxia, developmental delay, vision problems, hearing loss
- cutaneous abnormalities - alopecia, skin rash, candidiasis
- Links: OMIM
Congenital Adrenal Hyperplasia (CAH)
- Links: adrenal | adrenal abnormalities | genital abnormalities
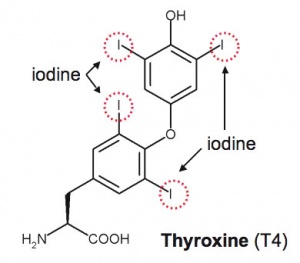
Congenital Hypothyroidism (CH)
- Links: thyroid
Congenital Toxoplasmosis
The causal agent of Toxoplasmosis is the protist Toxoplasma gondii (T. gondii). This unicellular eukaryote is a member of the phylum Apicomplexa, which includes other parasites responsible for a variety of diseases (malaria, cryptosporidiosis). The diagnosis and timing of an infection are diagnostically based on serological tests. During a period of acute maternal infection, transplacental transmission can occur, and the rate of congenital toxoplasmosis with risk for severe fetal varies from 15 to 68%, depending on gestational age. The transmission rate is highest in the later stages of pregnancy.
Congenital toxoplasmosis is characterized by a wide range of clinical manifestations; neurological, ophthalmological, and systemic involvement.
- Links: Toxoplasmosis | TORCH
Cystic Fibrosis (CF)
Cystic Fibrosis (CF) is a serious genetic disease due to abnormal chloride channel synthesis (cystic fibrosis transmembrane conductance regulator, CFTR), the impact occurs postnatally. Mucus accumulates mainly in the passages of the lungs and in the pancreas.
Galactosemia (GAL)
(Galactosaemia)
| Three different types: | 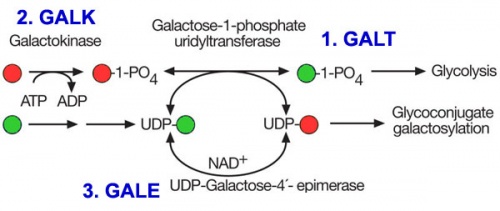
|
- Links: OMIM
Maple Syrup Urine Disease (MSUD)
Clinical features of MSUD are mental and physical retardation, feeding problems, and a maple syrup odor to the urine. The urine effects are due to the presence of keto acids of the branched-chain amino acids (branched-chain keto acid dehydrogenase enzyme subunits)
Four different types:
- type IA - caused by mutation in the E1-alpha subunit gene
- type IB - caused by a mutation in the E1-beta subunit gene
- type II - caused by defect in the E2 subunit gene
- type III - caused by defect in the E3 subunit
- Links: PubMed Health | OMIM
Medium-Chain Acyl-CoA Dehydrogenase Deficiency (MCAD)
MCAD deficiency is the most common inherited disorder of mitochondrial fatty acid oxidation in people from northern Europe. It is characterized by an intolerance to prolonged fasting and an inability to generate energy during periods of increased energy demand. The disorder can be severe to fatal in infants.
The other disease characteristics include: recurrent episodes of hypoglycemic coma with medium-chain dicarboxylic aciduria, impaired ketogenesis, and low plasma and tissue carnitine levels.
Gutherie test detected autosomal recessive metabolic disease affects about one in 10 000 people (UK). This mitochondrial protein is encoded by a nuclear gene on chromosome 1 (Gene map locus 1p31) and has a common mutation (985A>G) with a carrier rate of around one in 65.2.
Galactosylcerebrosidase Deficiency (GALC)
GALC deficiency (Krabbe disease, globoid cell leukodystrophy, galactosylceramidase deficiency) is a rare lysosomal disorder associated with mutation in the GALC gene (14q31) producing less galactosylceramidase. This lysosomal enzyme is required by glial cells (oligodendrocytes) in the nervous system to make myelin that insulates nerve cells. The disease has an autosomal recessive inheritance pattern. There is an even rarer infantile form caused by a mutation in the prosaposin (PSAP) gene (10q21-q22). The rarity of this disorder means that it may not be routinely tested everywhere.
There two main identified forms:
- An early-onset form - appears first months of life, often lethal before infant age 2 years.
- A late-onset form - appears in late childhood or early adolescence.
- Links: Image - autosomal recessive inheritance | Neural System Development | Neural Exam Movies | Inheritance Genetics
Tandem Mass Spectrometry
Tandem mass spectrometry (MS/MS) - can screen for PKU and many other diseases simultaneously (up to 21 metabolic diseases).[5]
Nuclear Medicine Renal Scan
DTPA Renal Scan - a test of renal function.
A radioactive compound is injected into the venous system, it then enters the renal system for excretion by the kidneys. A gamma camera can be used to track the compounds progress through the renal system.
Renal function measured:
- nephron function and perfusion
- ureter obstruction and trauma or damage
- renal artery stenosis
- hypertension
Endocrine
Congenital Hypothyroidism
Neonates born with congenital hypothyroidism (CH) typically have a normal appearance and no detectable physical signs. Thyroid hormone is required for normal postnatal neural (cognitive) development with newborn screening and thyroid therapy able to be begun within 2 weeks of birth.
The availability of a universal screening program for this hormonal abnormality varies from country to country.[6]
Congenital hypothyroidism can occur through either dysgenesis or agenesis of the thyroid gland development or abnormal thyroid hormone production. A false positive high thyroid stimulating hormone (TSH) can occur, due to the neonatal TSH surge that elevates TSH levels and causes T4 and T3 changes in the first 1 or 2 days after birth.
See also Iodine deficiency.
- Links: thyroid | iodine deficiency
Hearing
The incidence of significant permanent hearing loss is approximately 1-3/1000 newborns. Neonatal hearing screening is carried out in the USA, UK and in Australia (2002 NSW Statewide Infant Screening Hearing Program, SWISH) There is a general guide giving a timetable for a number of simple responses that a neonate should make if hearing has developed normally (More? Neonatal Hearing Check List).
State Wide Infant Screening Hearing Program (SWISH) a newborn hearing testing program using an automated auditory response technology (AABR). Program was introduced in NSW Australia in 2002 across 17 area health service coordinators. It is thought that in NSW 86,000 births/year = 86-172 babies potentially born with significant permanent hearing loss.
Automated Auditory Brainstem Response
(AABR) uses a stimulus which is delivered through earphones and detected by scalp electrodes. The test takes between 8 to 20 minutes and has a sensitivity 96-99%. The basis of a neonatal hearing test that uses a trigger stimulus delivered through earphones and subsequent brain electrical activity then detected by scalp electrodes. Then by computer analysis, averaging all the electrical activity following the trigger, peaks emerge reflecting signal passage activity through brain stem nuclei in the hearing central neural pathway. The infant test takes between 8 to 20 minutes, has a sensitivity 96-99%, and unlike other childhood auditory testing does not require a subject response. An alternative and simple test (pass/refer) used at a later stage is otoacoustic emission testing.
Otoacoustic Emission Testing
(OAE) The basis of a simple infant hearing test of the inner ear. A small probe containing both a speaker producing "clicks" and a microphone to detect cochlea responses is placed inside the ear canal. Acoustic energy produced by vibration of the hair cells in response to the clicks is detected by the microphone within the probe. A more complex test that can be used at an earlier stage is the automated auditory brainstem response.
Neonatal Hearing Check List
The timing and types of responses listed below reflect only a rough guide for the general population. Abnormalities in neurological, visual or motor skill development can also affect responses.
- Birth to 3 months - Reacts to loud sounds, Quiets to familiar voices or sounds, Makes cooing noises, Responds to speech by looking at speaker’s face
- 3 to 6 months - Turns eyes or head toward sounds, Starts to make speech-like sounds, Laughs and makes noises to indicate pleasure and displeasure
- 6 to 9 months - Babbles, ‘dada’‘ma-ma’‘baba’, Shouts/vocalises to get attention, Will often respond to ‘no’ and own name, Responds to singing and music
- 9 to 12 months - Imitates speech sounds of others, Understands simple words, eg ‘ball’,‘dog’, ‘daddy’, Turns head to soft sounds, First words emerge
- 12 to 18 months _ Appears to understand some new words each week, Follows simple spoken instructions, eg ‘get the ball’, Points to people, body parts or toys when asked, Continually learns new words to say although may be unclear
- 18 to 24 months - Listens to simple stories or songs, Combines two or more words in short phrases eg ‘more juice’
Hearing check list text based upon NSW Health Pamphlet - Why does my baby need a hearing check?
- Links: hearing test | hearing
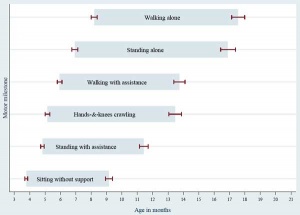
Neural
The newborn neuromuscular system can be initially assessed by 6 quick tests (posture, square window, arm recoil, popliteal angle, scarf sign and heel to ear). Later developmental assessment includes behaviour, reflexes (primitive and postural), muscular tone, and motor (gross, fine, co-ordination).
Neural examination can be carried out in the newborn and then later at 3 months, 6 months, 12 months and at 30 months of age.
There are several primitive reflexes (rooting, sucking reflexes, Moro, grasp) that change (are repressed) with development of the central nervous system.
Newborn Reflexes
|
|
|
| ||||||||||||
|
|
|
These movies were designed by PD Larsen and SS Stensaas, Utah School of Medicine.
Gene Tests
A new site developed by NIH "GeneTests" provides medical genetics information resources available at no cost to all interested persons. It contains educational information, a directory of genetic testing laboratories and links to other databases such as OMIM.
Genetic Testing Registry] (GTR) provides a central location for voluntary submission of genetic test information by providers.
Links: NIH - Genetic Testing Registry | GTR Overview
References
- ↑ Sampaio H, Wilcken B & Farrar M. (2018). Screening for spinal muscular atrophy. Med. J. Aust. , 209, 147-148. PMID: 30107765
- ↑ Ross LF & Clarke AJ. (2017). A Historical and Current Review of Newborn Screening for Neuromuscular Disorders From Around the World: Lessons for the United States. Pediatr. Neurol. , 77, 12-22. PMID: 29079012 DOI.
- ↑ 3.0 3.1 APGAR V. (1953). A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg , 32, 260-7. PMID: 13083014
- ↑ GUTHRIE R & SUSI A. (1963). A SIMPLE PHENYLALANINE METHOD FOR DETECTING PHENYLKETONURIA IN LARGE POPULATIONS OF NEWBORN INFANTS. Pediatrics , 32, 338-43. PMID: 14063511
- ↑ Cipriano LE, Rupar CA & Zaric GS. (2007). The cost-effectiveness of expanding newborn screening for up to 21 inherited metabolic disorders using tandem mass spectrometry: results from a decision-analytic model. Value Health , 10, 83-97. PMID: 17391418 DOI.
- ↑ Rose SR, Brown RS, Foley T, Kaplowitz PB, Kaye CI, Sundararajan S & Varma SK. (2006). Update of newborn screening and therapy for congenital hypothyroidism. Pediatrics , 117, 2290-303. PMID: 16740880 DOI.
Textbooks
- Enzyme-Replacement Therapies for Lysosomal Storage Diseases Ratko TA, Marbella A, Godfrey S, Aronson N. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Jan. PMID 23390670
Search PubMed: neonatal diagnosis | neonatal screening
Additional Images
- Gutherie card icon.jpg
Gutherie card
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- NIH PubMed Health Newborn Screening
- NIH Genetic Testing Registry (GTR) provides a central location for voluntary submission of genetic test information by providers. | GTR Overview
- Nemours Foundation Newborn Screening Tests
- The Children's Hospital at Westmead NSW Newborn Screening
- Secondary School Resource biotechnology online
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 20) Embryology Neonatal Diagnosis. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Neonatal_Diagnosis
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G