Birth
| Embryology - 25 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose. |
Introduction
Birth or parturition is a critical stage in development, representing in mammals a transition from direct maternal support of fetal development, physical expulsion and establishment of the newborns own respiratory, circulatory and digestive systems. These notes only cover the biological processes surrounding birth including fetal signaling changes and maternal signaling changes. Note that there is a growing worldwide trend in developed countries toward caesarean section delivery. There are a great number of comprehensive, scientific and general, books and articles that cover birth, childbirth or parturition. The time surrounding birth is known as the perinatal period.
The fetus is thought to initiate the labor process. Recent animal model studies show the maturing fetal lungs express steroid receptor coactivators 1 and 2 (SRC-1 and SRC-2) that induce production of Surfactant protein-A (SP-A) that is then secreted into amniotic fluid initiating parturition.[1]
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Birth <pubmed limit=5>Birth</pubmed> Search term: Childbirth <pubmed limit=5>Childbirth</pubmed> |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Textbooks
- Human Embryology (2nd ed.) Larson Chapter 15 pp471-488
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapter 7 pp129-167
- General Reading - Pregnancy and Childbirth S Kitzinger Doubleday, Sydney ISBN 0 86824 048 6
- Lecture - Birth
- Practical - Birth
History
| 1770 | 2010 | ||||
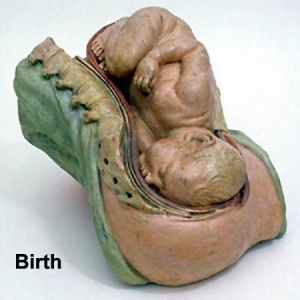
Teaching model of birth. |

Magnetic Resonance Imaging of birth. |
|
Gestation Period
Gestational Age GA
The American College of Obstetricians and Gynecologists Committee recently (2013) gave an opinion (no 579) definition of "term pregnancy".[5]
- "In the past, the period from 3 weeks before until 2 weeks after the estimated date of delivery was considered "term," with the expectation that neonatal outcomes from deliveries in this interval were uniform and good. Increasingly, however, research has shown that neonatal outcomes, especially respiratory morbidity, vary depending on the timing of delivery within this 5-week gestational age range. To address this lack of uniformity, a work group was convened in late 2012, which recommended that the label "term" be replaced with the designations early term (37 0/7 weeks of gestation through 38 6/7 weeks of gestation), full term (39 0/7 weeks of gestation through 40 6/7 weeks of gestation), late term (41 0/7 weeks of gestation through 41 6/7 weeks of gestation), and postterm (42 0/7 weeks of gestation and beyond) to more accurately describe deliveries occurring at or beyond 37 0/7 weeks of gestation. The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine endorse and encourage the uniform use of the work group's recommended"
The American Academy of Pediatrics Committee on Fetus and Newborn (2004) issued a policy statement "Age Terminology During the Perinatal Period"[10]
- "Gestational age GA (completed weeks): time elapsed between the first day of the last menstrual period and the day of delivery. If pregnancy was achieved using assisted reproductive technology, gestational age is calculated by adding 2 weeks to the conceptional age."
History
Historically, Franz Carl Naegele (1777-1851) developed the first scientific rule for estimating length of a pregnany. The median duration of gestation for first births from assumed ovulation to delivery was 274 days (just over 39 weeks). For multiple births, the median duration of pregnancy was 269 days (38.4 weeks).
- "...one should count back 3 months from the first day of the last menses, then add 15 days for primiparas or 10 days for multiparas, instead of using the common algorithm for Naegele's rule."[11]
Last Menstrual Period
The Last Menstrual Period (LMP), the menstrual period (menses) that occurs before a pregnancy, has been widely used clinically as a date to calculate clinical pregnancy development (GA, gestational age). Note that in humans this is approximately two weeks different from embryonic development, which begins at fertilisation around the mid-point of the menstrual cycle.
The interval between the beginning of the LMP and fertilisation can have a wide range (7 to 25 days). This variation can be due to both maternal (menstrual cycle timing and ovulation) and fetal (blastocyst implantation) effects. The calculation also requires an accurate maternal recall of LMP and can be affected by irregular menses, first-trimester vaginal bleeding, unrecognized spontaneous abortions, oral contraceptive use.
Ultrasound
Measurement of fetal size by ultrasound has been used more recently to accurately calculate pregnancy development. The ultrasound measurement tends to be more accurate in early development staging, by the third trimester there can be some individual variations in fetal growth and the effects of abnormalities or fetal growth restriction. Serial ultrasound measurements may identify these abnormal growth effects.
Birth Statistics
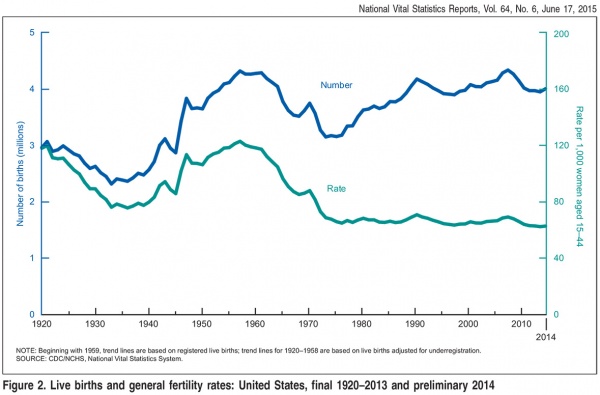
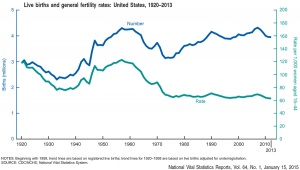
USA Live Births and Fertility Rates
The 2014 preliminary number of U.S. births was 3,985,924 an increase of 1% from 2013 (Data are based on 99.71% of 2014 births).[12]
| USA Live Births and general fertility rates (1920–2013)[13]
2013 Data[13] Number of births: 3,932,181 births were registered, down less than 1% from 2012.
|
|
2007 Data [14] Number of births: 4,317,119 Birth rate: 14.3 per 1,000 population Fertility rate: 69.5 births per 1000 women aged 15-44 years Percent born low birthweight: 8.2% Percent unmarried: 39.7%
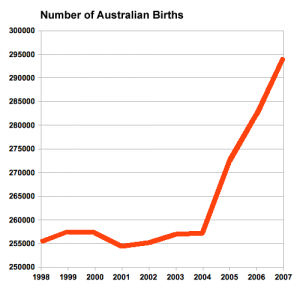
Australian Data
UK Data
|
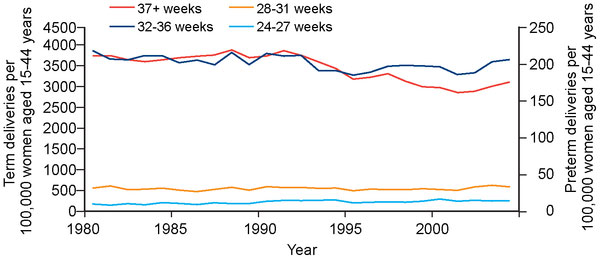
| Scotland - Spontaneous births per 100,000 women of reproductive age, 1980–2004.[15] |
Childbirth
- Parturition (Latin, parturitio = "childbirth") describes expelling the fetus, placenta and fetal membranes and is probably initiated by fetus not mother.
- Preterm birth - Risks of preterm birth in abnormal low birth weight (intrauterine growth restriction) and high (large for gestational age) categories are 2- to 3-fold greater than the risk among appropriate-for-gestational-age infants.
- Maternal labor - uterine contractions and dilation of cervix, process under endocrine regulation
- Placenta and fetal membranes - (Latin, secundina = "following") expelled after neonate birth
Uterine Myometrial Changes
- Smooth muscle fibers - hypertrophy not proliferation
- Stretching of myometrium - stimulates spontaneous muscular contraction, during pregnancy progesterone inhibits contraction
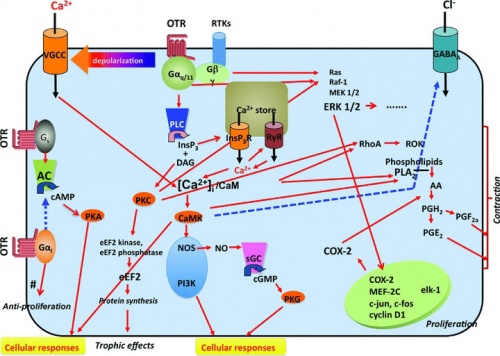
- Stimulating contraction - increased estrogen levels (placental secretion sensitizes smooth muscle), increased oxytocin levels (fetal oxytocin release- force and frequency of contraction), fetal pituitary prostaglandin production (estrogen and oxytocin stimulate endometrial production of prostaglandin)
| Hormones | Roles |
|---|---|
| Progesterone |
|
| Estrogens |
|
| Oxytocin |
|
| Prostaglandins |
|
| Endocrine | Birth |
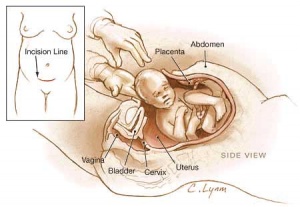
Oxytocin Receptor Pathways[17]
External Environment
- mainly shown in other species parturition occurs in peaceful undisturbed surroundings, stress may have an inhibitory effect on oxytocin release
- Most human births occur at night (peak at 3am) diurnal rhythm influence
Labor Stages
| Labour Stages | Changes | Time | Roles |
|---|---|---|---|
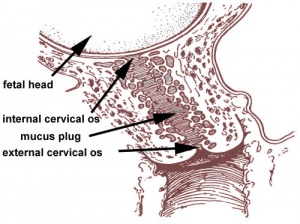
| Stage 1 | Dilatation | 7 to 12 hours longer for first child |
Uterine contractions 10 minutes apart, function to dilate cervix fetal membranes rupture releasing amnion. |
| Stage 2 | Expulsion | 20 to 50 minutes | Uterine contractions 2 to 3 minutes apart, function to push fetus through cervix and vagina. |
| Stage 3 | Placental | 15 minutes | Uterine contractions following child delivery expel placenta. Haematoma separates placenta from uterine wall, separation occurs at spongy layer of decidua basalis. |
| Stage 4 | Recovery | 2+ hours | Uterine contractions continue and myometrial contraction closes spiral arteries, also begins to reduce uterine volume. |
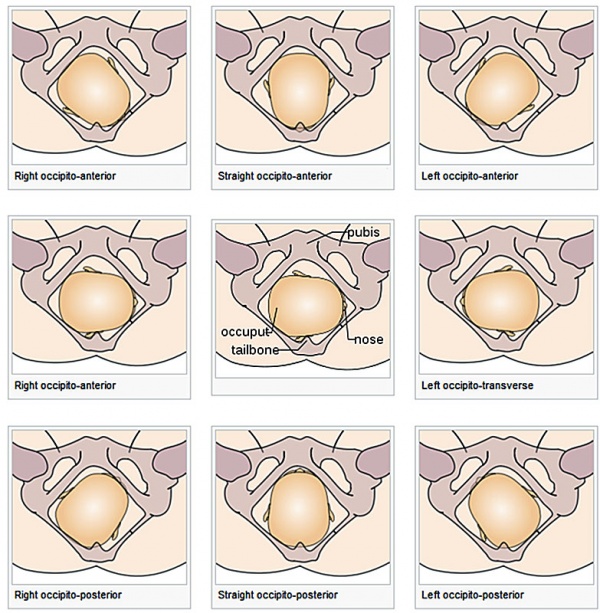
Presentation
Cephalic
Simplified views of fetal head positions, relative to maternal pelvis, in cephalic presentation at birth.
- Galletti (1770) Birth
Breech
- Galletti (1770) Breech Presentation
Historic Birth Models
About The Models - a series of models commissioned by Giuseppe Galletti (? - 1819) currently held in the Institute and Museum of the History of Science (Italy) Istituto e Museo di Storia della Scienza (IMSS). Giuseppe Galletti and others used terracotta and wax models that he had commissioned in Florence between 1770 and 1775 to train surgeons and midwives.
Birth Weights
The primary causes of VLBW are premature birth (born <37 weeks gestation, and often <30 weeks) and intrauterine growth restriction (IUGR), usually due to problems with placenta, maternal health, or to birth defects. Many VLBW babies with IUGR are preterm and thus are both physically small and physiologically immature.
| no colour | |||||||||||
| Birth weight (grams) | less 500 | 500 – 999 | 1,000 – 1,499 | 1,500 – 1,999 | 2,000 – 2,499 | 2,500 – 2,999 | 3,000 – 3,499 | 3,500 – 3,999 | 4,000 – 4,499 | 4,500 – 4,999 | 5,000 or more |
| Classification | |||||||||||
Newborn Homoeostasis
Newborn has to establish new functioning systems in a balanced and regulated manner (homoeostasis).
- lung function
- circulatory changes
- thermoregulation
- endocrine function
- nutrition
- gastrointestinal tract function
- waste
- kidney function
Glucocorticoids - have an important role in the preparation for birth, including involvement in lung and cardiac development, and the maturation of enzymes in a variety of pathways.
Respiration
- Lungs at birth collapsed and fluid-filled - replaced with air by powerful inspiratory movement and absorption through the alveoli
- Lung epithelia has to rapidly change from its prenatal secretory function to that of fluid absorbtion.
- initiated by a late fetal change in alveolar epithelial cell (AEC) chloride and fluid secretion to sodium and fluid absorption.
- absorption requires sodium-potassium ATPase (Na-K-ATPase) together with apical sodium entry mechanisms (Epithelial Sodium Channels, ENaC)
- Fetal thyroid hormone is thought to have a hormonal role in this developmental switch
- These changes and pressure also lead to the pulmonary sytem becoming activated and changes in the circulatory shunting that existed before birth.
- During the late fetal period regular fetal breathing movements (FBM) also occur preparing both the skeletomuscular sysyem and lungs mechanically for respiration.
- Respiratory Rate is higher than adult (30 breaths/minute).
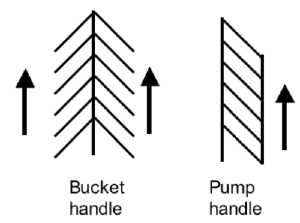
- Rib Orientation - Infant rib is virtually horizontal, allowing diaphragmatic breathing only. Adult rib orientation is oblique (both anterior and lateral views), allows for pump-handle and bucket handle types of inspiration.
The First Breath
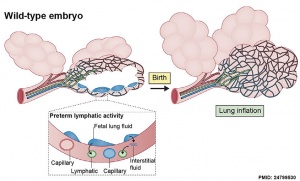
The exchange of lung fluid for air leads to:
- fall in pulmonary vascular resistance
- increase in pulmonary blood flow
- thinning of pulmonary arteries (stretching as lungs increase in size)
- blood fills the alveolar capillaries
- In the heart, pressure in the right side of the heart decreases and pressure in the left side of the heart increases (more blood returning from pulmonary).
See also the review; Clearance of lung liquid during the perinatal period[19] "At birth, the distal lung epithelium undergoes a profound phenotypic switch from secretion to absorption in the course of adaptation to air breathing."
Cardiovascular
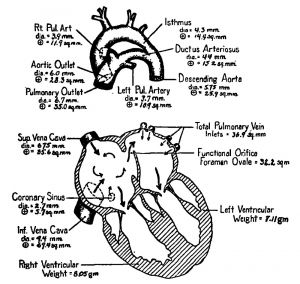
- Umbilical Vasculature - The umbilical blood vessel cavity is lost postnatally over the course of weeks to months after birth. The adult anatomical remnant of the umbilical vein between the umbilicus and liver is the ligamentum teres.
- foramen ovale - two separate forms of foramen ovale closure; functional and structural. Functional closure begins at the first breath and is rapid. Structural (anatomical) closure is much slower and generally occurs before the end of the first year.
- ductus arteriosus - a direct connection between the pulmonary trunk and the dorsal aorta. Postnatal closure occurs initially by by smooth muscle contraction and begins at the first breath and is rapid, completed within the first day (about 15 hr after birth). Anatomical closure is much slower occuring by 2–3 weeks after birth (33% of infants), by 2 months (90% of infants) and by 1 year (99% of infants). The adult anatomical remnant of the ductus arteriosus is the ligamentum arteriosum.
- ductus venosus - connects portal and umbilical blood to the inferior vena cava. Functional closure occurs postnatally within hours. Structural closure commences days after birth and completes by 18 to 20 days. The adult anatomical remnant of the ductus venosus is the ligamentum venosum (a dorsal fissure on the liver).
Premature Birth

| Year | < 34 weeks % | 34-36 weeks % | total preterm % |
| 1990 | 3.3 | 7.3 | 10.6 |
| 1995 | 3.3 | 7.7 | 11 |
| 2000 | 3.4 | 8.2 | 11.6 |
| 2005 | 3.6 | 9.1 | 12.7 |
Data: Prevention of preterm birth: a renewed national priority[22]
Australia Recommendations
Perinatal care at the borderlines of viability: a consensus statement based on a NSW and ACT consensus workshop, February 2005[23] and 2007[24]
- less than 23 weeks survival is minimal and the risk of major morbidity is so high that initiation of resuscitation is not appropriate.
- 23 weeks active treatment may be discussed, but would be discouraged in NSW/ACT neonatal intensive care units.
- 23 to 25 weeks otherwise normal infant, there is an increasing obligation to treat. However, it is acceptable medical practice not to initiate intensive care if parents so wish, following appropriate counselling.
- 24 weeks antenatal transfer to a tertiary centre for fetal reasons is indicated. The option of non-initiation of intensive care/resuscitation should be offered.
- 25 weeks active treatment is usually offered, but the option of non-initiation of intensive care/resuscitation (presence of adverse fetal factors such as twin-to-twin transfusion, intrauterine growth restriction or chorioamnionitis) should also be discussed.
- 26 weeks or more otherwise normal infant the obligation to treat is very high, and treatment should generally be initiated unless there are exceptional circumstances.
- "A grey zone between 23(0) and 25(6) weeks of gestation was identified and agreed upon. In this grey zone, while there was an increasing obligation to treat, it was acceptable not to initiate intensive care following appropriate counselling with parents. Important areas identified before birth, were continuing communication between the perinatal team and parents, a review of choice with continued counselling, decision support and empathy."[24]
Postterm Birth
Postterm pregnancy is a ((GA) of 42 weeks or beyond and has risks for both infant and mother (see review[25]).
- incidence of stillbirth increases from GA 39 weeks onwards
- incidence of stillbirth has a sharp rise after GA of 40 weeks
Birth Induction
Maternal and Neonatal Outcomes of Elective Induction of Labor
AHRQ Evidence Report 2009 (USA)
- Induction of labor is on the rise in the USA, increasing from 9.5 percent in 1990 to 22.1 percent in 2004.
- Although, it is not entirely clear what proportion of these inductions are elective (i.e. without a medical indication), the overall rate of induction of labor is rising faster than the rate of pregnancy complications that would lead to a medically indicated induction. However, the maternal and neonatal effects of induction of labor are unclear. Many studies compare women with induction of labor to those in spontaneous labor. This is problematic, because at any point in the management of the woman with a term gestation, the clinician has the choice between induction of labor and expectant management, not spontaneous labor. Expectant management of the pregnancy involves nonintervention at any particular point in time and allowing the pregnancy to progress to a future gestational age. Thus, women undergoing expectant management may go into spontaneous labor or may require indicated induction of labor at a future gestational age.
- Randomized controlled trials suggest that elective induction of labor at 41 weeks of gestation and beyond may be associated with a decrease in both the risk of cesarean delivery and of meconium-stained amniotic fluid. The evidence regarding elective induction of labor prior to 41 weeks of gestation is insufficient to draw any conclusion. There is a paucity of information from prospective RCTs examining other maternal or neonatal outcomes in the setting of elective induction of labor. Observational studies found higher rates of cesarean delivery with elective induction of labor, but compared women undergoing induction of labor to women in spontaneous labor and were subject to potential confounding bias, particularly from gestational age. Such studies do not inform the question of how elective induction of labor affects maternal or neonatal outcomes. Elective induction of labor at 41 weeks of gestation and potentially earlier also appears to be a cost-effective intervention, but because of the need for further data to populate these models our analyses are not definitive. Despite the evidence from the prospective, RCTs reported above, there are concerns about the translation of such findings into actual practice, thus, there is a great need for studying the translation of such research into settings where the majority of obstetric care is provided.[26]
- Links: NCBI Bookshelf - Full Report | | search pubmed
Symphysiotomy
A clinical procedure (operation) carried out to increase pelvic outlet size and to permit vaginal delivery of a baby, the surgical procedure involves dividing the cartilage of the symphysis pubis.[27][28] This can be employed for a number of birth related issues including: lack of caesarean option, obstructed birth, breech birth and shoulder dystonia.
The operation can lead to transient maternal pelvic instability. A recent Cochrane study looking at "the effectiveness and safety of symphysiotomy versus alternative options for obstructed labour in various clinical situations" identified no randomized trials of symphysiotomy.[29]
Shoulder Dystocia
Term describing a birth condition where the fetal bisacromial diameter is greater than the maternal pelvic inlet antero-posterior diameter. This leads to the fetal anterior shoulder becoming impacted behind the maternal pubic symphysis. More simply, the shoulder becomes "stuck" during birth.[30] This condition generally has a low incidence[31], but can occur in up to 3% of all births and there are a range of clinical procedures employed to overcome the problem depending on the degree and stage of birth. Effects associated with this clinical condition include fetal clavicle (collar bone) breakage and brachial plexus damage.[32][33]
It is thought that the recent trend for increasing maternal obesity has in turn led to increasing fetal macrosomy that has increased shoulder dystocia and fetal clavicle breakage.
Clinical procedures: suprapubic pressure with normal downward traction on fetal head, McRoberts maneuver, Wood's screw maneuver, Posterior arm extraction and Procto-episiotomy.
- Links: American Academy of Family Physicians - Shoulder Dystocia | Australia - The Royal Women’s Hospital | search pubmed
Instrumental Assistance
Birth - cephalic presentations
The two main forms of instrumental assistance to expedite vaginal delivery with either vacuum or forceps. There can be associated complications for both mother and infant with these procedures, that influence assistance selection.[34]
Ventouse
A vacuum device (metal or rubber-type cup with tubing attached) used to assist the delivery of a infant when the second stage of labour has not progressed adequately.
Forceps
A surgical instrument similar to a pair of tongs used to mechanically assist the delivery of a infant. The modern instrument was historically developed several hundred years ago to grab and manoeuvre the fetus through the birth canal.
Neonatal Testing
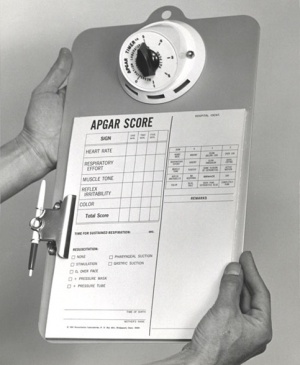
Apgar Test
A historic neonatal test designed by Dr Virginia Apgar[35] used in nearly all maternity clinics to assess the newborn infants well being assigned scores for each of 5 indicators: Heart Rate, Respiratory Effort, Reflex Irritability, Muscle Tone, Colour Measured at one and five minutes after birth the Score values are totalled for all indicators: 7-10 is considered normal, 4-7 may require resuscitative measures, 3 and below require immediate resuscitation. In recent years there has been some controversy of the relevance and accuracy of some of the criteria used in this test, though many feel it is still an invaluable initial assessment tool particularly where medical services are limited.
- Measured at one and five minutes after birth.
- The Score values are totalled for all indicators
- 7 to 10 is considered normal
- 4 to 7 may require resuscitative measures
- 3 and below require immediate resuscitation
| Indicator | Score 0 | Score 1 | Score 2 |
| Activity (muscle tone) |
Limp; no movement | Some flexion of arms and legs | Active motion |
| Pulse (heart rate) |
No heart rate | Fewer than 100 beats per minute | At least 100 beats per minute |
| Grimace (reflex response) |
No response to airways being suctioned | Grimace during suctioning | Grimace and pull away, cough, or sneeze during suctioning |
| Appearance (color) |
The baby's whole body is completely bluish-gray or pale | Good color in body with bluish hands or feet | Good color all over |
| Respiration (breathing) |
Not breathing | Weak cry; may sound like whimpering, slow or irregular breathing | Good, strong cry; normal rate and effort of breathing |
| Table data[35] Apgar test - Measured at one and five minutes after birth, the score values are totalled for all indicators: | |||
| Total Score: | 3 and below require immediate resuscitation | 4 to 7 may require resuscitative measures | 7 to 10 is considered normal |
|---|---|---|---|
- Links: Apgar test
Guthrie Test
A blood screening test developed by Dr Robert Guthrie (1916-95) at University of Buffalo.[36] The test is carried out on neonatal (newborn) blood detecting markers for a variety of known disorders (phenylketonuria (PKU), hypothyroidism and cystic fibrosis). In the Australian states of NSW and Victoria, the Guthrie Cards are currently stored indefinitely.
- Links: Guthrie test
Abnormalities
There are many birth associated abnormalities, only a few examples are listed below. In particular the perinatal period is a time when fetal systems that have either not yet been functional (respiratory, gastrointestinal, neural) or are extensively remodelled (cardiovascular, placental). There are also a number of maternal issues.
Mark Hill (talk) 11:12, 26 March 2019 (AEDT) This section is currently being version updated from ICD-10 to ICD-11.
Uterine Rupture
Maternal uterine rupture is defined as an anatomic separation of the uterine muscle with or without symptoms and has adverse consequences for both mother and infant. AN NIH consensus conference[37]identified a increased risk of uterine rupture in women who have a trial of labor compared to elective repeat cesarean delivery. "There have been no reported maternal deaths due to uterine rupture. Overall, 14 to 33 percent of women will need a hysterectomy when the uterus ruptures. Approximately 6 percent of uterine ruptures will result in perinatal death. This is an overall risk of intrapartum fetal death of 20 per 100,000 women undergoing trial of labor. For term pregnancies, the reported risk of fetal death with uterine rupture is less than 3 percent. Although the risk is similarly low, there is insufficient evidence to quantify the neonatal morbidity directly related to uterine rupture."
- ICD: O71.0 Rupture of uterus before onset of labour | O71.1 Rupture of uterus during labour, Rupture of uterus not stated as occurring before onset of labour | Uterus Abnormalities | Uterus Development
Amniotic Fluid Embolism
(AFE) Clinical term for a rare obstetric emergency in which conceptus material (amniotic fluid, fetal cells, hair, or other fetal debris) enter the maternal circulation from the placenta and lead to an allergic reaction followed by maternal cardiorespiratory collapse. Amniotic fluid can enter maternal circulation through tears in the uterus or cervix during labour and delivery, or through partial separation of the placenta.
A recent international study[38] has attempted to standardise how AFE data is collected and recommended:
- Comparisons of AFE incidence estimates should be restricted to studies using similar methodology. The recommended approaches would be either population-based database studies using additional criteria to exclude false positive cases, or tailored data collection using existing specific population-based systems.
- Comparisons of AFE incidence between and within countries would be facilitated by development of an agreed case definition and an agreed set of criteria to minimise inclusion of false positive cases for database studies.
- Groups conducting detailed population-based studies on AFE should develop an agreed strategy to allow combined analysis of data obtained using consistent methodologies in order to identify potentially modifiable risk factors.
- Future specific studies on AFE should aim to collect information on management and longer-term outcomes for both mothers and infants in order to guide best practice, counselling and service planning.
Labor Abnormalities
- Premature Labor - occurs 7 -10% in humans, contributes 75% perinatal mortalities
- Underdeveloped Systems - particularly respiratory, surfactant, hyaline membrane disease (see respiratory development lecture)
Placental Abnormalities
- placenta accreta - abnormal adherence, with absence of decidua basalis
- placenta percreta - villi penetrate myometrium
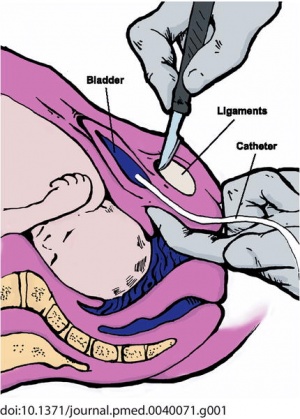
- placenta previa - placenta overlies internal os of uterus, abnormal bleeding, cesarian delivery
Breech Delivery

|

|
- Historically, breech-born children were called agrippi, meaning "delivered with difficulty" (aegre parti).
- Breech position - occurs in about 3% of fetuses when buttocks or lower limb are presented to the birth canal rather than normal cephalic (head-first) position (presentation).
- Associated increased - perinatal mortality, perinatal morbidity, recurrence in successive siblings
Current research suggests that genetically that both men and women delivered in breech presentation at term could also contribute to an increased risk of breech delivery in their offspring.[39]
Meconium Aspiration Syndrome
- meconium is formed from gut and associated organ secretions as well as cells and debris from the swallowed amniotic fluid.
- Meconium accumulates during the fetal period in the large intestine (bowel). It can be described as being a generally dark colour (green black) , sticky and odourless.
- Normally this meconium is defaecated (passed) postnatally over the first 48 hours and then transitional stools from day 4.
- Abnormally this meconium is defaecated in utero, due to oxygen deprivation and other stresses. Premature discharge into the amniotic sac can lead to mixing with amniotic fluid and be reswallowed by the fetus. This is meconium aspiration syndrome and can damage both the developing lungs and placental vessels.
Necrotizing Enterocolitis
Occurs postnatally in mainly in premature and low birth weight infants (1 in 2,000 - 4,000 births). The underdeveloped gastointestinal tract appears to be susceptible to bacteria, normally found within the tract,to spread widely to other regions where they damage the tract wall and may enter the bloodstream.
References
- ↑ Gao L, Rabbitt EH, Condon JC, Renthal NE, Johnston JM, Mitsche MA, Chambon P, Xu J, O'Malley BW & Mendelson CR. (2015). Steroid receptor coactivators 1 and 2 mediate fetal-to-maternal signaling that initiates parturition. J. Clin. Invest. , 125, 2808-24. PMID: 26098214 DOI.
- ↑ Ngo TTM, Moufarrej MN, Rasmussen MH, Camunas-Soler J, Pan W, Okamoto J, Neff NF, Liu K, Wong RJ, Downes K, Tibshirani R, Shaw GM, Skotte L, Stevenson DK, Biggio JR, Elovitz MA, Melbye M & Quake SR. (2018). Noninvasive blood tests for fetal development predict gestational age and preterm delivery. Science , 360, 1133-1136. PMID: 29880692 DOI.
- ↑ Arya S, Mulla ZD & Plavsic SK. (2018). Outcomes of Women Delivering at Very Advanced Maternal Age. J Womens Health (Larchmt) , , . PMID: 30016194 DOI.
- ↑ Broekman BFP, Wang C, Li Y, Rifkin-Graboi A, Saw SM, et al. (2014) Gestational Age and Neonatal Brain Microstructure in Term Born Infants: A Birth Cohort Study. PLoS ONE 9(12): e115229. doi:10.1371/journal.pone.0115229
- ↑ 5.0 5.1 . (2013). ACOG Committee Opinion No 579: Definition of term pregnancy. Obstet Gynecol , 122, 1139-40. PMID: 24150030 DOI.
- ↑ Myklestad K, Vatten LJ, Magnussen EB, Salvesen KÅ & Romundstad PR. (2013). Do parental heights influence pregnancy length?: A population-based prospective study, HUNT 2. BMC Pregnancy Childbirth , 13, 33. PMID: 23383756 DOI.
- ↑ De Bie HMA, Oostrom KJ, Boersma M, Veltman DJ, Barkhof F, et al. (2011) Global and Regional Differences in Brain Anatomy of Young Children Born Small for Gestational Age. PLoS ONE 6(9): e24116. doi:10.1371/journal.pone.0024116 PLoS ONE
- ↑ Does Birth Weight Influence Physical Activity in Youth? A Combined Analysis of Four Studies Using Objectively Measured Physical Activity PMC3020226
- ↑ Hadfield RM, Lain SJ, Simpson JM, Ford JB, Raynes-Greenow CH, Morris JM & Roberts CL. (2009). Are babies getting bigger? An analysis of birthweight trends in New South Wales, 1990-2005. Med. J. Aust. , 190, 312-5. PMID: 19296812
- ↑ Engle WA. (2004). Age terminology during the perinatal period. Pediatrics , 114, 1362-4. PMID: 15520122 DOI.
- ↑ Mittendorf R, Williams MA, Berkey CS & Cotter PF. (1990). The length of uncomplicated human gestation. Obstet Gynecol , 75, 929-32. PMID: 2342739
- ↑ Hamilton BE, Martin JA, Osterman MJK, Curtin SC. Births: Preliminary data for 2014. National vital statistics reports; vol 64 no 6. Hyattsville, MD: National Center for Health Statistics. 2015. http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_06.pdf
- ↑ 13.0 13.1 Martin JA, Hamilton BE, Osterman MJK, et al. Births: Final data for 2013. National vital statistics reports; vol 64 no 1. Hyattsville, MD: National Center for Health Statistics. 2015. http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf
- ↑ USA National Vital Statistics System - Birth Data
- ↑ Norman JE, Morris C & Chalmers J. (2009). The effect of changing patterns of obstetric care in Scotland (1980-2004) on rates of preterm birth and its neonatal consequences: perinatal database study. PLoS Med. , 6, e1000153. PMID: 19771156 DOI.
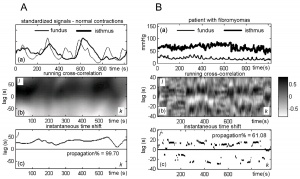
- ↑ Pierzynski P, Oczeretko E, Laudanski P & Laudanski T. (2007). New research models and novel signal analysis in studies on preterm labor: a key to progress?. BMC Pregnancy Childbirth , 7 Suppl 1, S6. PMID: 17570166 DOI.
- ↑ Viero C, Shibuya I, Kitamura N, Verkhratsky A, Fujihara H, Katoh A, Ueta Y, Zingg HH, Chvatal A, Sykova E & Dayanithi G. (2010). REVIEW: Oxytocin: Crossing the bridge between basic science and pharmacotherapy. CNS Neurosci Ther , 16, e138-56. PMID: 20626426 DOI.
- ↑ Dewerchin M. (2014). Lymphatics help baby take first breath. J. Exp. Med. , 211, 745. PMID: 24799530 DOI.
- ↑ Barker PM & Olver RE. (2002). Invited review: Clearance of lung liquid during the perinatal period. J. Appl. Physiol. , 93, 1542-8. PMID: 12235057 DOI.
- ↑ Windle WF. Physiology of the Fetus. (1940) Saunders, Philadelphia.
- ↑ MacKay DF, Smith GC, Dobbie R & Pell JP. (2010). Gestational age at delivery and special educational need: retrospective cohort study of 407,503 schoolchildren. PLoS Med. , 7, e1000289. PMID: 20543995 DOI.
- ↑ Damus K. (2008). Prevention of preterm birth: a renewed national priority. Curr. Opin. Obstet. Gynecol. , 20, 590-6. PMID: 18989136 DOI.
- ↑ Lui K, Bajuk B, Foster K, Gaston A, Kent A, Sinn J, Spence K, Fischer W & Henderson-Smart D. (2006). Perinatal care at the borderlines of viability: a consensus statement based on a NSW and ACT consensus workshop. Med. J. Aust. , 185, 495-500. PMID: 17137454
- ↑ 24.0 24.1 Kent AL, Casey A & Lui K. (2007). Collaborative decision-making for extreme premature delivery. J Paediatr Child Health , 43, 489-91. PMID: 17535182 DOI.
- ↑ Galal M, Symonds I, Murray H, Petraglia F & Smith R. (2012). Postterm pregnancy. Facts Views Vis Obgyn , 4, 175-87. PMID: 24753906
- ↑ Caughey AB, Sundaram V, Kaimal AJ, Cheng YW, Gienger A, Little SE, Lee JF, Wong L, Shaffer BL, Tran SH, Padula A, McDonald KM, Long EF, Owens DK & Bravata DM. (2009). Maternal and neonatal outcomes of elective induction of labor. Evid Rep Technol Assess (Full Rep) , , 1-257. PMID: 19408970
- ↑ Verkuyl DA. (2007). Think globally act locally: the case for symphysiotomy. PLoS Med. , 4, e71. PMID: 17388656 DOI.
- ↑ Ersdal HL, Verkuyl DA, Björklund K & Bergström S. (2008). Symphysiotomy in Zimbabwe; postoperative outcome, width of the symphysis joint, and knowledge, attitudes and practice among doctors and midwives. PLoS ONE , 3, e3317. PMID: 18846216 DOI.
- ↑ Hofmeyr GJ & Shweni PM. (2010). Symphysiotomy for feto-pelvic disproportion. Cochrane Database Syst Rev , , CD005299. PMID: 20927742 DOI.
- ↑ Allen RH. (2007). On the mechanical aspects of shoulder dystocia and birth injury. Clin Obstet Gynecol , 50, 607-23. PMID: 17762413 DOI.
- ↑ Rahman J, Bhattee G & Rahman MS. (2009). Shoulder dystocia in a 16-year experience in a teaching hospital. J Reprod Med , 54, 378-84. PMID: 19639928
- ↑ Andersen J, Watt J, Olson J & Van Aerde J. (2006). Perinatal brachial plexus palsy. Paediatr Child Health , 11, 93-100. PMID: 19030261
- ↑ Chauhan SP, Cole J, Laye MR, Choi K, Sanderson M, Moore RC, Magann EF, King HL & Morrison JC. (2007). Shoulder dystocia with and without brachial plexus injury: experience from three centers. Am J Perinatol , 24, 365-71. PMID: 17566948 DOI.
- ↑ O'Mahony F, Hofmeyr GJ & Menon V. (2010). Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev , , CD005455. PMID: 21069686 DOI.
- ↑ 35.0 35.1 APGAR V. (1953). A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg , 32, 260-7. PMID: 13083014
- ↑ GUTHRIE R & SUSI A. (1963). A SIMPLE PHENYLALANINE METHOD FOR DETECTING PHENYLKETONURIA IN LARGE POPULATIONS OF NEWBORN INFANTS. Pediatrics , 32, 338-43. PMID: 14063511
- ↑ NIH Consensus Development Conference on Vaginal Birth After Cesarean: New Insights. March 8–10, 2010, Bethesda, Maryland. Statement
- ↑ Knight M, Berg C, Brocklehurst P, Kramer M, Lewis G, Oats J, Roberts CL, Spong C, Sullivan E, van Roosmalen J & Zwart J. (2012). Amniotic fluid embolism incidence, risk factors and outcomes: a review and recommendations. BMC Pregnancy Childbirth , 12, 7. PMID: 22325370 DOI.
- ↑ Nordtveit TI, Melve KK, Albrechtsen S & Skjaerven R. (2008). Maternal and paternal contribution to intergenerational recurrence of breech delivery: population based cohort study. BMJ , 336, 872-6. PMID: 18369204 DOI.
Reviews
Articles
MacKay DF, Smith GC, Dobbie R & Pell JP. (2010). Gestational age at delivery and special educational need: retrospective cohort study of 407,503 schoolchildren. PLoS Med. , 7, e1000289. PMID: 20543995 DOI.
Books
- Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition. Geneva: World Health Organization; 2015. Available from: http://www.ncbi.nlm.nih.gov/books/NBK326678/
- National Collaborating Centre for Women's and Children's Health (UK). Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. London: National Institute for Health and Care Excellence (UK); 2014 Dec. (NICE Clinical Guidelines, No. 190.) Available from: http://www.ncbi.nlm.nih.gov/books/NBK290736/
- National Collaborating Centre for Mental Health (UK). Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance: Updated edition. Leicester (UK): British Psychological Society; 2014 Dec. (NICE Clinical Guidelines, No. 192.) Available from: http://www.ncbi.nlm.nih.gov/books/NBK305023/
Search Pubmed
Search Pubmed: Birth | Parturition | Fetal Changes Birth
Birth Terms
| Birth Terms | ||
|---|---|---|
| ||
|
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- The Journal of Perinatal Education
- Australia - Victorian Department of Health Neonatal ehandbook - structured approach to the clinical management of conditions regularly encountered by health professionals caring for newborns.
- World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. Published 2012.
- Video - Human birth (1973) - Shows birth complications which students rarely experience in the delivery room. Includes instructions on vertex delivery, spontaneous breech delivery, assisted breech delivery, extraction cesarean delivery and multiple births.
| System Links: Introduction | Cardiovascular | Coelomic Cavity | Endocrine | Gastrointestinal Tract | Genital | Head | Immune | Integumentary | Musculoskeletal | Neural | Neural Crest | Placenta | Renal | Respiratory | Sensory | Birth |
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 25) Embryology Birth. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Birth
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G