Bone Histology
| Embryology - 25 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
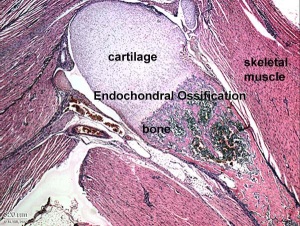
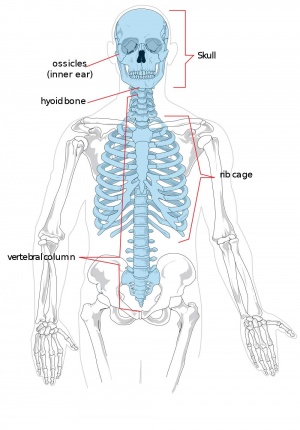
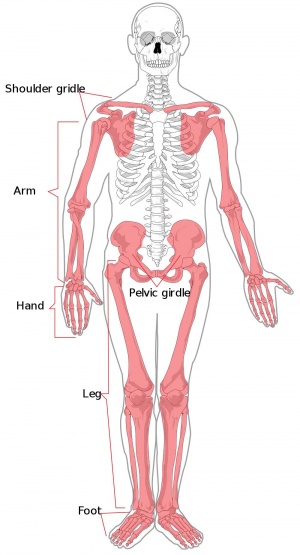
Our adult skeleton forms from a larger number of developmental elements that are replaced and fuse. In development there are 2 separate signaling pathways for pattern formation and the formation of bone itself. Furthermore bone formation can be divided into 2 specific forms that occur in anatomically different regions. This practical class will describe the development and structure of bone and finish with a study of abnormalities associated with bone.
The image shown to the left shows a histological section through the developing lower limb at the level of a developing joint (knee), surrounding the developing bone are skeletal muscles and connective tissue of the limb.
Note: This current page contains both additional information and images to the practical class set. These are provided for educational information and study purposes only. For more development background see the Science Lecture - Musculoskeletal Development and notes on Bone Development.
Page also provides further histology background information for Medicine phase 1 Ageing and Endings Practical Virtual Slides.
Objectives
- Understand the general microanatomy of bone
- Understand bone cell types (location, structure, function)
- Understand the histology of compact and spongy bone
- Understand the 2 forms of developmental bone formation
Textbook
Histology and Cell Biology: An Introduction to Pathology, A.L. Kierszenbaum, 2002 - Connective Tissue, Chapter 4 pp118-129; Osteogenesis, Chapter 5 pp131-145
Slides
UNSW Virtual Slidebox Virtual Slidebox Phase 1
Virtual Slidebox of Histology Decalcified rib, bone marrow | Developing bone | Paget's disease of bone
Bone Structure
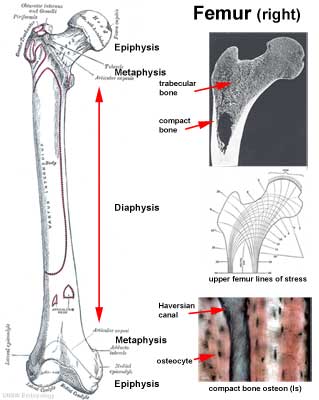
Terminology
- Diaphysis - shaft
- Epiphysis - expanded ends
- Metaphysis - connecting region (between diaphysis and epiphysial line)
- Medullary Cavity - (marrow) cavity within the bone.
More? Terms
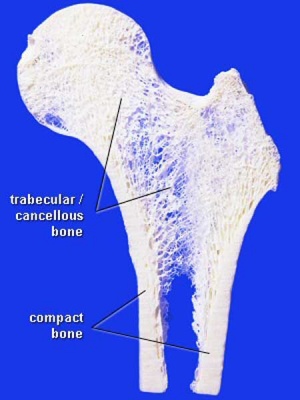
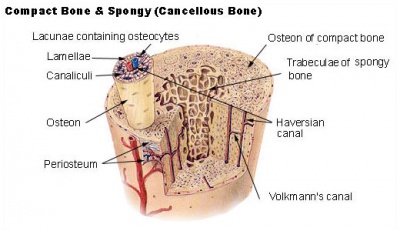
Compact Bone
- (dense) no spaces or hollows in the bone matrix visible to the eye.
- forms the thick-walled tube of the shaft (or diaphysis) of long bones, which surrounds the marrow cavity (or medullary cavity). A thin layer of compact bone also covers the epiphyses of long bones.
Trabecular Bone
- (cancellous or spongy bone) consists of delicate bars (spicules) and sheets of bone, trabeculae
- branch and intersect to form a sponge-like network
- ends of long bones (or epiphyses) consist mainly of trabecular bone.
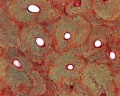
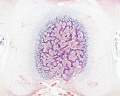
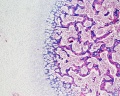
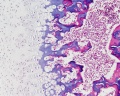
trabecular - overview (Stain - Haematoxylin Eosin)
trabecular - low (Stain - Haematoxylin Eosin)
trabecular - med (Stain - Haematoxylin Eosin)
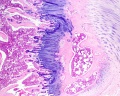
Periosteum
The embryonic origin of this layer is still controversial. The connective tissue coating covering the surface of bone, except at the articular surfaces, consisting of two distinct main layers with sub-layers.[1]
|

|
Endosteum
Connective tissue lining inner surface of bone.
Bone Growth
- Appositional growth occurs at either the periosteum (outer surface), or the endosteum (inner surface).
- Osteoblasts secrete osteoid, a pre-bone material composed mainly of type I collagen that becomes mineralized.
- Early bone matrix deposited in development and during repair is woven rather than lamellar in appearance and structure.
- In development, there are 2 distinct types of bone formation (intramembranous and endochondral)
Bone Cells
Osteoblasts
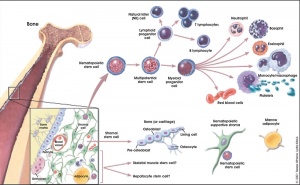
- derive from osteogenic stem cells the osteoprogenitor cells that differentiate to form pre-osteoblast then osteoblasts maturing to an osteocyte
- osteoprogenitor cells - "resting cell" line the inner and outer surfaces of bone
- mononuclear cells that differentiate from mesenchymal progenitors
- differentiation controlled by several transcriptional factors (Runx2) and signaling cascades.
- support osteoclast differentiation (by up-regulation of RANKL expression)
Osteocytes
- mature bone-forming cells embedded in lacunae within the bone matrix
- osteoblasts and osteocytes - secrete organic matrix of bone (osteoid), converted into osteocytes when become embedded in matrix (which calcifies soon after deposition)
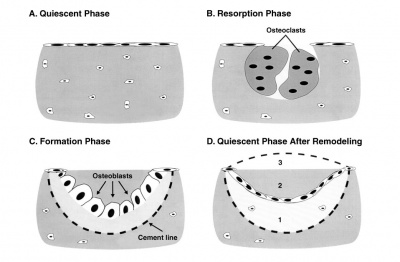
Osteoclasts
- bone-resorbing multi-nucleated macrophage-like cells
- origin- fusion of monocytes or macrophages, Blood macrophage precursor, Attach to bone matrix
- seal a small segment of extracellular space (between plasma membrane and bone surface), HCl and lysosomes secreted into this space by osteoclasts dissolves calcium phosphate crystals (give bone rigidity and strength)
- Resorptive bay - (Howship's lacuna) shallow bay lying directly under an osteoclast.
- do not mistake for megakaryocytes, found in bone marrow not associated with bone matrix.
- megakaryocytes are also multi-niucleated and form platelets
- tartrate-resistant acid phosphate (TRAP)–positive
- differentiate from monocyte/macrophage lineage by stimulation by two essential cytokines
- macrophage colony-stimulating factor (M-CSF)
- receptor activator of nuclear factor κB ligand (RANKL)
Bone Marrow
- red marrow - mainly haematopoietic (myeloid) tissue, newborn has all red marrow
- yellow marrow - mainly fat cells, found in diaphysis region of long bones
- stromal cells - all other support cells not involved in haematopoiesis
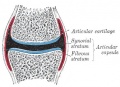
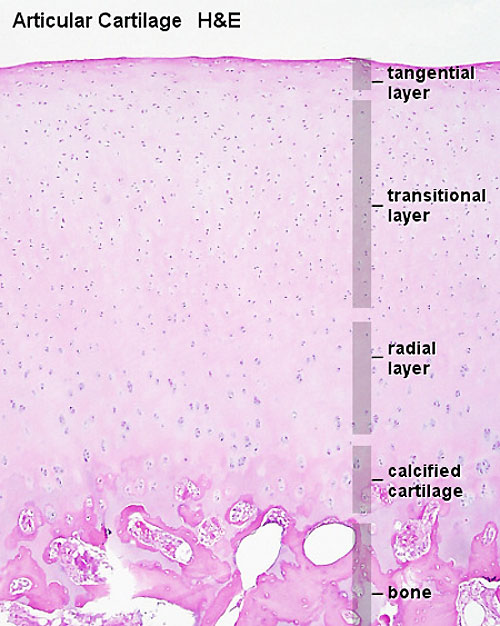
Chondroblasts and Chondrocytes
- immature and mature cartilage forming cells located at articular cartilage regions.
- Interstitial growth - occurs mainly in immature cartilage. Chondroblasts in existing cartilage divide and form small groups of cells (isogenous groups) which produce matrix to become separated from each other by a thin partition of matrix.
- Appositional growth - occurs also in mature cartilage. Mesenchymal cells surrounding the cartilage in the deep part of the perichondrium (or the chondrogenic layer) differentiate into chondroblasts.
- Links: Cartilage Histology
Bone Matrix
The bone matrix has 2 major components.
- Organic portion composed of mainly collagen Type 1 (about 95%) and amorphous ground substance.
- Inorganic portion (50% dry weight of the matrix) composed of hydroxyapatite crystals, calcium, phosphorus, bicarbonate, nitrate, Mg, K, Na.
- storage calcium and phosphate
- regulate blood calcium levels
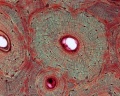
Haversian System
|
|
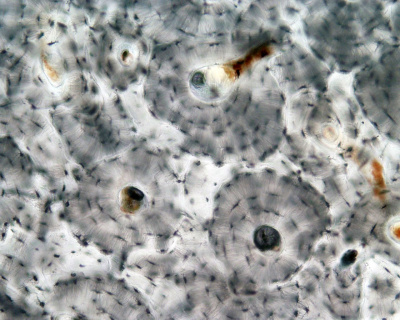
|
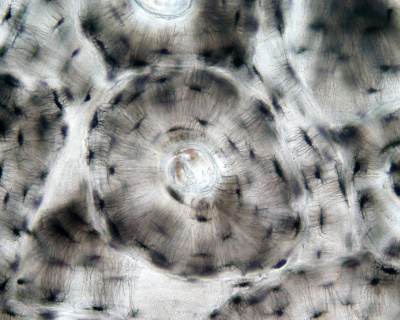
|
| Low Power (x10) | High Power (x20) |
Lamellae
- concentric - surrounding each Haversian System
- interstitial - bony plates that fill in between the haversian systems.
- circumferential - layers of bone that underlie the periosteum and endosteum
Cells
- osteocytes extending cytoplasmic processes into canaliculi
- Additional Histology images: low | medium | high
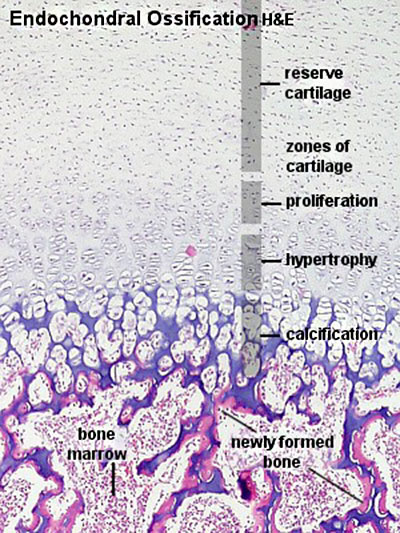
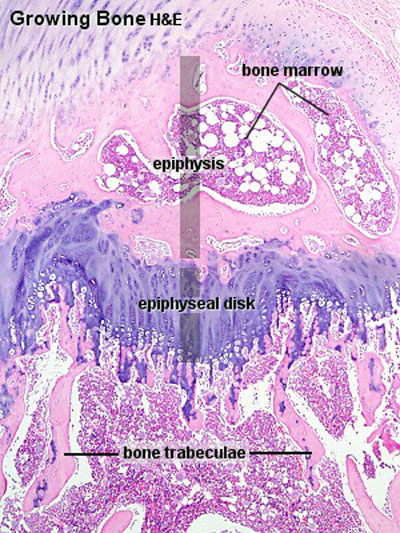
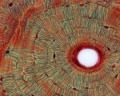
Endochondral ossification
Endochondral ossification slides: Developing bone | Bone, Developing (LS, Femur) Cat H&E
Dev Biology - endochondral ossification | endochondral ossification animation
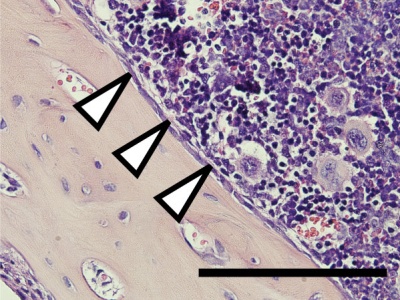
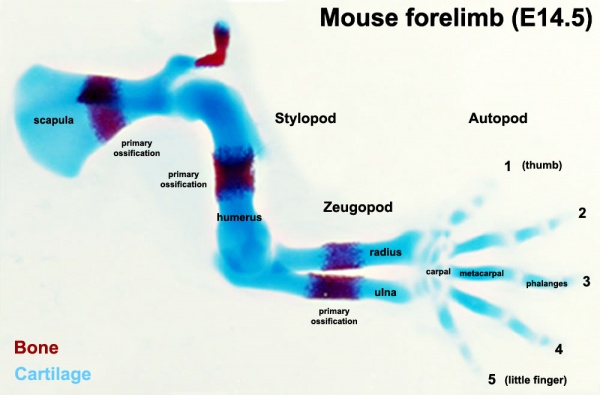
Primary ossification
Primary ossification in mouse limb (E14.5)
Gallery
- Bone Histology: Cartilage Histology | Histology Stains | Histology | cartilage | bone | bone timeline
- Trabecular bone trabecular | lamellar | trabecular - overview HE | trabecular - low HE | trabecular - med HE
- Endochondral ossification primary ossification | endochondral ossification
- Intramembranous ossification intramembranous - VG low | intramembranous - VG high | intramembranous - HE low | intramembranous - HE high
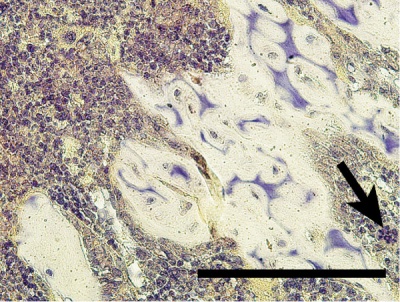
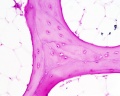
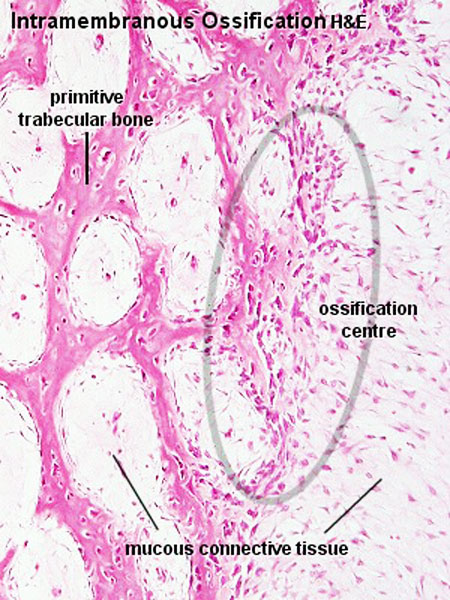
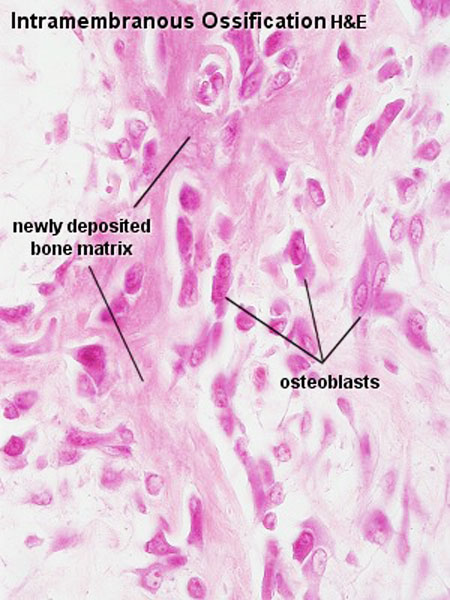
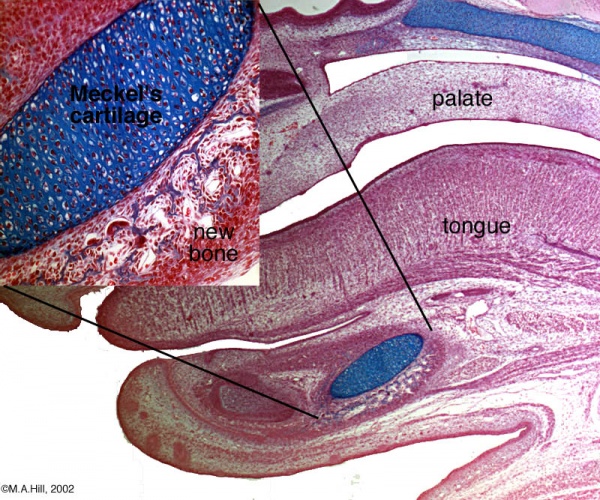
Intramembranous Ossification
Intramembranous ossification slides: Head (Neonatal) Rat H& Van Gieson
- Bone Histology: Cartilage Histology | Histology Stains | Histology | cartilage | bone | bone timeline
- Trabecular bone trabecular | lamellar | trabecular - overview HE | trabecular - low HE | trabecular - med HE
- Endochondral ossification primary ossification | endochondral ossification
- Intramembranous ossification intramembranous - VG low | intramembranous - VG high | intramembranous - HE low | intramembranous - HE high
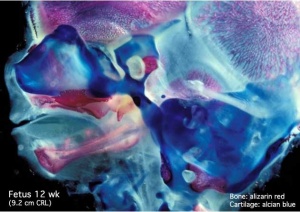
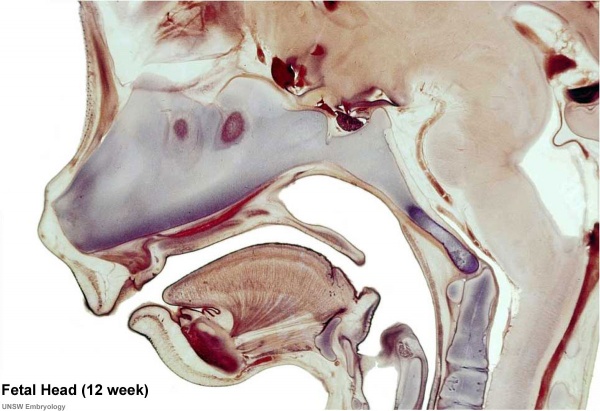
Human Fetal Head (12 week)
Histology Stains
Alizarin Red
- an anthraquinone derivative used to identify calcium in tissue sections
- calcium forms an Alizarin Red S-calcium complex in a chelation process and the end product is also birefringent.
- reaction can also identify magnesium, manganese, barium, strontium, and iron may interfere
- these elements usually in too low concentration to interfere with the staining
H&E
- acronym for hematoxylin and eosin stain
- hematoxylin - basic dye which colors basophilic structures with blue-purple hue (nucleus, DNA, RNA)
- eosin Y - acidic alcohol-based which colors eosinophilic structures bright pink (cytoplasm, extracellular matrix, protein)
H&Van Gieson
- Van Gieson's Stain is a mixture of picric acid and acid fuchsin used for differential staining of collagen and other connective tissue.
- Nuclei - stains brownish black to black
- Collagen (fibrous connective tissue) - stains pink or deep red
- Muscle, Cytoplasm, RBC and Fibrin - stains yellow
- Links: Histology Stains
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
References
Mackie EJ, Ahmed YA, Tatarczuch L, Chen KS & Mirams M. (2008). Endochondral ossification: how cartilage is converted into bone in the developing skeleton. Int. J. Biochem. Cell Biol. , 40, 46-62. PMID: 17659995 DOI.
Other Textbooks
- Anatomy of the Human Body (H. Gray, 1918.) historical anatomy text Osteology
- Molecular Biology of the Cell Bone Is Continually Remodeled by the Cells Within It | Image: Figure 22-52. Deposition of bone matrix by osteoblasts | Image: Figure 22-56. The development of a long bone
- Molecular Cell Biology Mutations in Collagen Reveal Aspects of Its Structure and Biosynthesis
- The Cell- A Molecular Approach Steroid Hormones and the Steroid Receptor Superfamily
- Clinical Methods: The History, Physical, and Laboratory Examinations 100. Alkaline Phosphatase and Gamma Glutamyltransferase
- Endocrinology: An Integrated Approach by Nussey, S.S. and Whitehead, S.A. Endocrinology: Definition and causes of osteoporosis
- Developmental Biology 6th ed. by Gilbert, Scott F. Figure 14.13. Schematic diagram of endochondral ossification | Aging: The Biology of Senescence
Search
- Pubmed ossification
Terms
| Bone Terms | ||
|---|---|---|
Bone Development
| ||
|
- canaliculus - (plural, canaliculi) small channel in the bone matrix in which an osteocyte process lies and communicates with other osteocytes and the Haversian canal.
- haematopoiesis (Greek, haima = "blood"; poiesis = "to make") the process of blood cell formation.
- Haversian canal - the central canal of an osteon (Haversian system) in compact bone, within which blood vessels and nerves travel throughout the bone.
- Haversian system - (osteon) the historic name for the functional unit of compact bone. Consists of a central canal (Haversian canal) surrounded by lamellar bone matrix within which osteocytes reside.
- Howship's lacuna - (resorptive bay) the historic name for the shallow bay or cavity lying directly under an osteoclast. This is the site of bone matrix resorption.
- lacuna - (Latin, lacuna = “ditch, gap” diminutive form of lacus = “lake”) lacunae is the plural, cavity in bone or cartilage for cell.
- lamellar bone - the highly organized strong bone matrix deposited in concentric sheets with a low proportion of osteocytes. Many collagen fibers parallel to each other in the same layer.
- osteon - (Haversian system) the functional unit of compact bone. Consists of a central canal (Haversian canal) surrounded by lamellar bone matrix within which osteocytes reside.
- resorptive bay - (Howship's lacuna) the shallow bay or cavity lying directly under an osteoclast. This is the site of bone matrix resorption.
- suture - in the skull a form of articulation where the contiguous margins of the bones are united by a thin layer of fibrous tissue.
- woven bone - the first deposited weaker bone matrix with many osteocytes and a matrix disorganized structure. Replaced by lamellar bone. Seen in developing, healing and bone disease.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 25) Embryology Bone Histology. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Bone_Histology
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G